Protein Clumping Best Blocked Using Specific Compounds at Distinct Disease Stages, Model Suggests
A mathematical model created to more effectively prevent protein clumping, widely thought to underlie diseases like Parkinson’s, found that different potential treatments work best at different disease stages.
As such, this model may help in designing and timing the use of therapies against protein aggregates, and in testing them in clinical trials for Parkinson’s, Alzheimer’s, and other diseases.
The study, “Optimal control strategies for inhibition of protein aggregation,” was published in the journal Proceedings of the National Academy of Sciences.
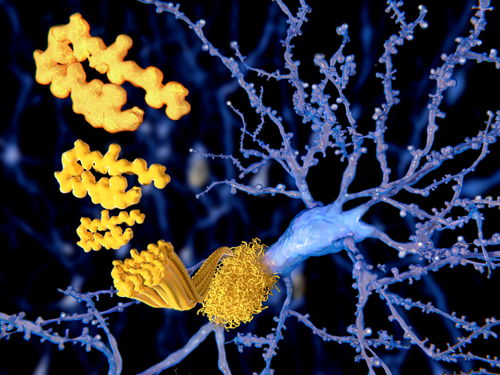
Protein aggregation is a complex process involving multiple microscopic steps. It starts with an event called primary nucleation, in which misfolded (altered shape) proteins clump together to form fibrils, which then elongate. This first step proceeds slowly, potentially taking up to several decades.
A later event is called secondary nucleation. Here, aggregation speeds up and exponential growth occurs, with existing clumps promoting the formation of new ones. This faster phase is associated with evident disease, and a potential for rapid progression.
Aggregates of misfolded proteins are fairly established treatment targets of Parkinson’s, Alzheimer’s, and other diseases. However, finding a therapy combination and dose regimen that is both effective and of limited toxicity — so that side effects don’t make it unusable — has been challenging.
Recent studies suggest that compounds known as molecular inhibitors (blockers) and targeting different types of aggregates, might be an effective approach. Examples include the anti-cancer treatment bexarotene (marketed as Targretin by Ortho Dermatologists for cutaneous T-cell lymphoma) and antibodies.
To help find the right balance between suppressing aggregation and avoiding toxicity, researchers at the Harvard John A. Paulson School of Engineering and Applied Sciences developed a predictive treatment model that combined the physics of protein aggregation with so-called control theory, which assesses the behavior of dynamic systems in mathematics and engineering.
To test their model, the scientists analyzed data from a disease model, the worm Caenorhabditis elegans, that can be engineered to form amyloid-beta clumps that eventually paralyze the worms. Specifically, they looked at the efficacy of bexarotene and a compound known as DesAb29-36. Both these compounds inhibit the aggregation of amyloid-beta — the main component of senile plaques in Alzheimer’s and of normal aging — but at different steps: bexarotene targets primary nucleation, while DesAb29-36 works to block secondary nucleation.
Investigators found that the optimal approach depends on whether a potential treating is targeting primary or secondary nucleation, and on whether the compound can be effective at non-toxic levels. Compound concentration plays a key role, as low amounts require longer periods of administration. However, if exceeding a critical threshold, it turns toxic so that side effects outweigh benefits.
When they analyzed earlier studies in this worm model of amyloid-beta aggregation, scientists found benefits with increasing but low doses of bexarotene in terms of worm movement at disease onset (larval stages). As levels of bexarotene rose, they found it had the opposite effect on worm mobility, indicating the existence of an optimal dose.
Consistent with the effect of bexarotene on primary nucleation, the model predicted that this therapy would be most effective early in the disease course. It had a demonstrated lack of benefits in adult worms.
In turn, the model predicted that DesAb29-36 would be most effective if administered at a later stage of aggregation, in line with its targeting secondary nucleation.
“Our results pose and answer the question of the link between the molecular basis of protein aggregation and optimal strategies for inhibiting it, opening up avenues for the design of rational therapies to control pathological protein aggregation,” the researchers wrote.
In a university news release written by Leah Burrows, Thomas C. T. Michaels, PhD, a lead study author, said the team’s approach is “unique” and “will allow people to test the efficacy of different compounds against aggregation under optimal conditions.”
“From these optimal conditions,” Michaels added, “one could then extrapolate optimal conditions for a [clinical] trial. So, in this sense, our work could help seed potential trials.”
Added L Mahadevan, PhD, the study’s senior author and a professor of applied mathematics at Harvard University: “Our research highlights the importance of understanding the relationship between the chemical kinetics of protein misfolding, the mechanisms by which drugs inhibit protein aggregation, and the timing of their administration.”
All this, he said, “could have important implications for intervention protocols to prevent pathological protein aggregation.”






