Psychosis in Parkinson’s Linked to Volume Changes in Specific Area of Brain, Study Says
Psychosis and cognitive impairment in patients with Parkinson’s disease may be linked to structural changes in the brain, namely a decrease in volume of an area that controls memory formation, a study suggests.
The study, “Hippocampal subfield atrophy in patients with Parkinson’s disease and psychosis,” was published in the Journal of Neural Transmission.
Psychosis, which usually manifests as visual hallucinations, is one of the most frequently observed non-motor symptoms of Parkinson’s disease.
More than 50 percent of Parkinson’s patients will experience psychosis in their lifetimes, and the condition is associated with poor quality of life and more use of healthcare resources.
The causes underlying psychosis in Parkinson’s disease remain unclear, but some studies suggest it may be linked to structural and functional alterations of the hippocampus, a brain region that plays a key role in memory formation.
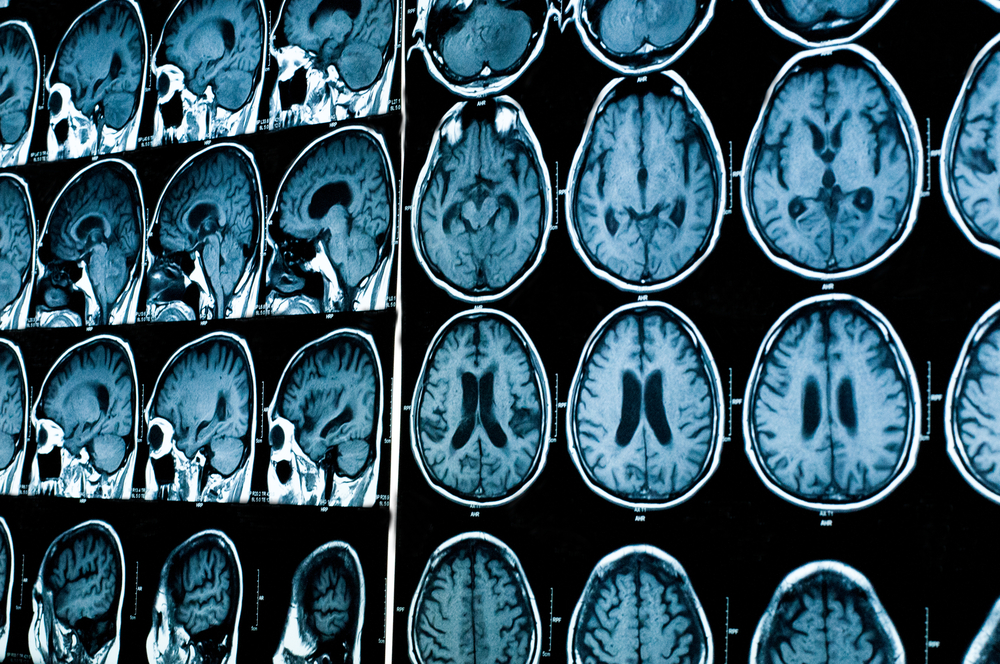
Using magnetic resonance imaging (MRI), researchers analyzed the hippocampus of 51 Parkinson’s patients without psychosis, 42 Parkinson’s patients with psychosis, and 48 healthy people matched by age, gender, and education, used as controls.
Patients were recruited from the National Institute of Mental Health and Neurosciences in Bangalore, India.
Additional parameters analyzed included participants’ overall cognitive performance, measured using the Montreal Cognitive Assessment Scale (MoCA), and frontal executive functions — the skills a person uses to plan, organize and complete tasks — evaluated using the frontal assessment battery (FAB), which assesses the brain’s frontal lobe function.
Overall cognitive performance was significantly higher in healthy controls than in Parkinson’s patients both with and without psychosis. There were no significant differences in cognition between the Parkinson’s patients, regardless of whether they had psychosis or not.
Discuss the latest research news in the Parkinson’s News Today forum!
FAB scores were also significantly lower in both groups of Parkinson’s patients than controls, highlighting an impairment in executive functions in patients both with and without psychosis.
Researchers observed that the overall volume of the hippocampus was reduced in Parkinson’s patients with psychosis compared with healthy controls, and that the volumes of different subzones in the hippocampus of these patients correlated with psychosis severity and cognitive functions.
However, Parkinson’s patients with psychosis had increased volume of a specific region within the hippocampus called the hippocampal fissure. The higher the volume in this area, the lower the capacity of visual memory and visuospatial functions.
Mouse studies have previously demonstrated that an increase in hippocampal fissure volume is highly correlated with a decrease in overall hippocampal volume, and can be considered a radiological hallmark of ongoing brain atrophy.
“We demonstrated that the trajectory of psychosis severity could be mapped using hippocampal subfield volumes,” the researchers wrote.
These results support the involvement of specific hippocampal regions in psychosis and cognitive impairment in Parkinson’s disease.






