Mutation Plays a Role in Fatty Plaque Formation in Brain, Study Suggests
Written by |
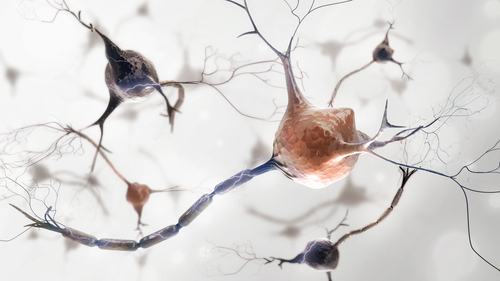
A common Parkinson’s gene mutation plays a role in the formation of fatty plaque in the brain that can destroy nerve cells controlling movement, a study suggests.
The research, “GBA1 deficiency negatively affects physiological α-synuclein tetramers and related multimers,” was published in the Proceedings of the National Academy of Sciences.
Five to 10 percent of Parkinson’s patients have a mutation of the GBA1 gene. It generates an enzyme responsible for breaking down a large fat molecule into smaller ones called ceramides.
Fat molecules are the glue that helps proteins maintain a complex design in cell membranes. The GBA1 enzyme is supposed to ensure that the glue is strong enough to hold the mosaic together.
In addition to ensuring cell membrane integrity, the enzyme is also responsible for the normal functioning of the cell’s recycling system.
Johns Hopkins researchers used the gene editing technology CRISPR-Cas9 to remove the enzyme from lab-grown brain cells. As expected, its depletion led to an accumulation of a fatty molecule called glucosylceramide and increased cell stress.
Strikingly, when glucosylceramide levels rose, the number of stable alpha-synuclein tetramers — a hallmark of Parkinson’s disease — fell.
Researchers then treated the modified brain cells with Zavesca (miglustat), an approved therapy for the treatment of Gaucher disease type 1 that prevents fatty molecule buildups.
The treatment led to cells recovering their levels of alpha-synuclein tetramers. This suggested that high levels of glucosylceramide destabilize the cell membrane mix. The result is alpha-synuclein tetramers falling out of the mosaic and breaking into single alpha-synucleins, the researchers said.
To further assess the potential of targeting GBA1 to treat Parkinson’s, the team used brain cells collected from a patient with a mutated GBA1 gene. These cells had lower than normal GBA1 activity and higher than normal levels of glucosylceramide. The result was an accumulation of alpha-synuclein monomers.
Once more, treatment with Zavesca promoted alpha-synuclein stability and tetramer formation, while preventing the accumulation of alpha-synuclein fibrils that is characteristic of Parkinson’s disease. In addition, the researchers showed that increasing the amount of functional GBA1 with gene therapy also promoted alpha-synuclein stability.
“We believe this study gives us a better understanding of the effects of GBA1 mutation and its role in the development and progress of Parkinson’s disease,” Dr. Han Seok Ko, an associate professor of neurology at the Johns Hopkins University School of Medicine’s Institute for Cell Engineering, said in a press release.
The team plans to continue study the enzyme’s effect on alpha-synuclein and nerve cell health.





