Gut Fungi Not Linked to Parkinson’s Development
Written by |
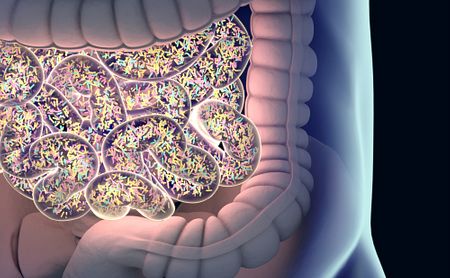
While scientists continue to shed light on a connection between gut bacteria and Parkinson’s disease, one study has found that gut fungi appear not to contribute to the neurodegenerative disorder.
This result might serve as a useful warning against investing in potentially futile anti-fungal treatments for people with Parkinson’s, researchers said.
Titled “The Gut Mycobiome in Parkinson’s Disease,” the study was published in the Journal of Parkinson’s Disease.
The study’s conclusion might sound underwhelming, but it addresses a need within both the Parkinson’s community and funding organizations to publish negative results in addition to positive ones.
By knowing what won’t, or is unlikely to work, researchers can better avoid devoting their valuable and often scarce resources toward projects with little chance of success.
A team of scientists from the University of British Columbia, in Canada, had sought to determine if any differences in fungal populations in the gut might associate with aspects of Parkinson’s disease. To that end, they examined stool samples from 95 Parkinson’s patients and 57 healthy individuals (controls).
“The gut microbiome has been increasingly implicated in Parkinson’s disease,” the researchers wrote, “however, most existing studies employ bacterial-specific sequencing, and have not investigated non-bacterial microbiome constituents.”
The stool samples contained little gut fungus in general. The researchers found enough fungi to analyze in 106 of the 152 participants — 64 with Parkinson’s and 42 healthy controls. What existed differed little between those with and without Parkinson’s, the results showed.
The saccharomyces yeast — a type of single-celled fungus — appeared as the most prevalent type of fungus in all participants, accounting for more than 50% of all fungi found in the study. Although saccharomyces includes many species, it is best known for those involved in baking and brewing.
The overall low amount of fungi relative to bacteria in the samples suggested to the investigators that they find the gut a less hospitable environment.
“The data are an important piece in the puzzle of understanding the overall role of the gut microbiome in [Parkinson’s],” Silke Appel-Cresswell, MD, the study’s lead investigator, said in a related press release.
Patients can “rest assured that gut fungal overgrowth, or dysbiosis, is likely not a contributing factor to any of their [Parkinson’s] symptoms, both motor and non-motor,” added Appel-Cresswell, of the faculty of medicine at the University of British Columbia.
Specifically, no associations were found with any motor, cognitive, or gastrointestinal features of the disease.
“The gut microbiome in [Parkinson’s] continues to be an exciting field of research where we are just at the beginning of unraveling potential mechanisms. It will be important to publish negative results as well as positive findings along with detailed methods to have a realistic reflection of the data in the literature to accelerate discovery,” Appel-Cresswell concluded.


