New Technique Can Mitigate Parkinson’s Disease Nerve Cell Transplant Side Effects
 A completely new preclinical technique developed by researchers at Lund University in Sweden involves analysis of tissue from patients to show exactly what happens in Parkinson’s disease (PD) patients who have nerve function restored as a result of nerve cell transplants. The scientists have also identified the reason why many such transplant patients develop serious side effects manifesting in the form of involuntary movements.
A completely new preclinical technique developed by researchers at Lund University in Sweden involves analysis of tissue from patients to show exactly what happens in Parkinson’s disease (PD) patients who have nerve function restored as a result of nerve cell transplants. The scientists have also identified the reason why many such transplant patients develop serious side effects manifesting in the form of involuntary movements.
The investigators note that while Parkinson’s disease treatments have improved over the past several decades, the problem of serious side effects — caused by both medication and the transplantation of nerve cells — remains.
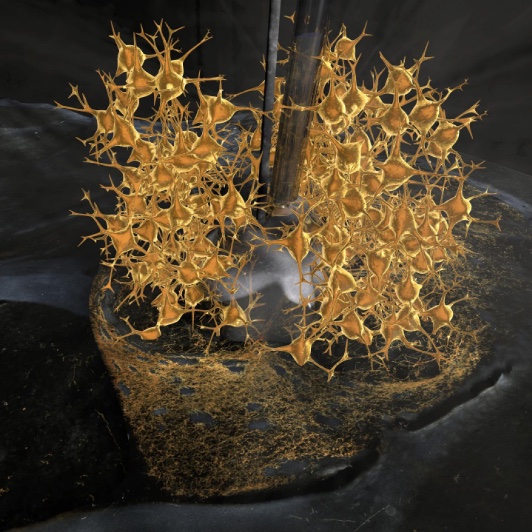
Photo Caption – The illustration shows a histological section from three dopamine cell transplants in the rat brain affected by Parkinson’s disease. An artistic illustration shows how the transplanted cells are controlled by a new gene, so that they can be steered externally using a drug. This allows the nerve cells’ function to be studied with unrivaled exactitude in the brain using an implanted electrode. With the help of this technique, the Lund researchers have been able to increase the dopamine cell transplant’s function to a level where the animal has been completely restored. Furthermore, they have also used this technique to identify the exact signaling pathway that gives rise to the most common side effects that patients experience as a result of this treatment. Photo Credit: Bengt Mattsson, Lunds universitet
Parkinson’s is caused by a deficit of nerve cells that produce the neurotransmitter dopamine in the brain, and one of the newer treatment methods is transplantation of dopamine-producing cells into affected parts of the brain. Unfortunately, while some patients have been completely restored after such a transplant, others have experienced onset of involuntary movements known as dyskinesias as a side effect of the transplant therapy. Dyskinesias are also a common side effect of medication treatment using the Parkinson’s drug L-DOPA, and the reason why has been unknown until now.
For several years, researcher and Postdoctoral Research Fellow in Molecular Neuromodulation at the Lund University Faculty Of Medicine Tomas Björklund and a team of investigator colleagues have been working to develop a completely new technique for studying how transplanted nerve cells actually function after they’re transplanted into the brains of persons afflicted with
Parkinson’s disease. An artificial receptor the scientists place on the surface of transplanted cells is activated by a specially designed drug that controls the cells’ release of dopamine. In animal testing, the investigators have shown that this method can be used to control transplanted dopamine-producing cells’ activity in the brain, and when the dopamine-producing cells are activated, the animal’s function is almost completely restored.
 “It is like a remote control for the brain. Using this new technique, we can now either close down the transplanted cells completely or increase their activity,” says Björklund in a release. “Now we can control very closely when and how the cells function when transplanted into the area of the brain affected by the disease.” (Photo: Lund University)
“It is like a remote control for the brain. Using this new technique, we can now either close down the transplanted cells completely or increase their activity,” says Björklund in a release. “Now we can control very closely when and how the cells function when transplanted into the area of the brain affected by the disease.” (Photo: Lund University)
The Lund researchers explain their findings and methodologies in an Open Access report funded by the European Research Council published in the journal Neuron entitled “DREADD Modulation of Transplanted DA Neurons Reveals a Novel Parkinsonian Dyskinesia Mechanism Mediated by the Serotonin 5-HT6 Receptor” (Neuron, May 2016 DOI: 10.1016/j.neuron.2016.04.017), coauthored by Björklund with Patrick Aldrin-Kirk, Andreas Heuer, Gang Wang, Bengt Mattsson, Martin Lundblad, and Malin Parmar.
The coauthors note that interest in the therapeutic potential of cell replacement in Parkinson’s disease (PD) in particular has re-emerged with the new EU-funded clinical trial using fetal cells, the development of optimized and efficient differentiation protocols for human embryonic stem cells (hESCs), and the emerging plans for the use of hESCs or induced pluripotent stem cells (iPSCs) in clinical trials in PD patients (https://www.gforce-pd.com/). They also reference pioneering clinical trials, performed over the last decades using dopamine (DA) neuroblasts from fetal mesencephalon (still considered the gold-standard DA cell replacement in PD) that have been encouraging but also have raised significant concerns regarding the above-mentioned significant proportion of patients who have developed abnormal involuntary movements induced by the graft (graft-induced dyskinesias, or GID).
They point to recent studies showing that these GIDs are dependent of serotonergic neurotransmission and can be suppressed by drugs acting on inhibitory autoreceptors located on the serotonin neurons. However, they say the functional link between the serotonin system and dysregulated DA neurotransmission causing dyskinesias still remains elusive and raise concerns for future clinical trials, mainly due to all attempts to reproduce this side effect in an authentic and clinically relevant animal model having failed so far.
The goal of the DREADD Modulation study was to explore the mechanism underlying induction of GIDs using a novel rat model where DA neurons from Cre-expressing donor rats are transplanted to the striatum in Parkinsonian rats. The transplants are subsequently transduced to express, selectively within the grafted DA neurons, a novel bimodal pair of chemogenetic receptors, and the researchers have for the first time been able to generate a rat model where DA neurons derived from fetal midbrain neuroblasts can be selectively modulated using a bimodal chemogenetic approach.
“We have now been able to map exactly what it is that makes nerve cell transplantation effective as a treatment,” says Tomas Björklund in a Lund release. “We have had access to unique patient material from a patient who has had this type of cell transplant and have also found a very high level expression of the receptor that causes the side effects. The discovery is important, as in future clinical treatment using cell transplantation can be carried out with a considerably reduced risk of side effects, and the effect of the treatment can be enhanced.”
“There are advanced plans in many parts of the world to carry out new clinical studies with nerve cell transplants from both fetuses and stem cells against Parkinson’s disease, which means that it’s now more relevant than ever to identify the underlying mechanisms in the brain”‘ Björklund concludes.
For more information about the study, contact: Tomas Björklund, researcher at Lund University, Telephone: + 46 46 222 68 36, Mobile: +46 72-5112277
Sources:
Lund University
Neuron






