Scientists Discover How to Turn Stem Cells Into Dopaminergic Neurons
Written by |
A new method for turning specific human stem cells, called pluripotent stem cells, into neurons that can produce dopamine — the signaling molecule, essential for controlling movement, that is missing in patients with Parkinson’s disease — has now been developed by researchers in the U.S.
“Scientists have been trying hard to generate these neurons from human pluripotent stem cells to study Parkinson’s disease and develop better therapies,” Jian Feng, PhD, professor at the University at Buffalo and the study’s senior author, said in a university press release.
“We have succeeded in making A9 dopamine neurons from human induced pluripotent stem cells. It means that we can now generate these neurons from any [Parkinson’s disease patient] to study their disease,” he added.
The study, “Generation of human A9 dopaminergic pacemakers from induced pluripotent stem cells,” was published in the journal Molecular Psychiatry.
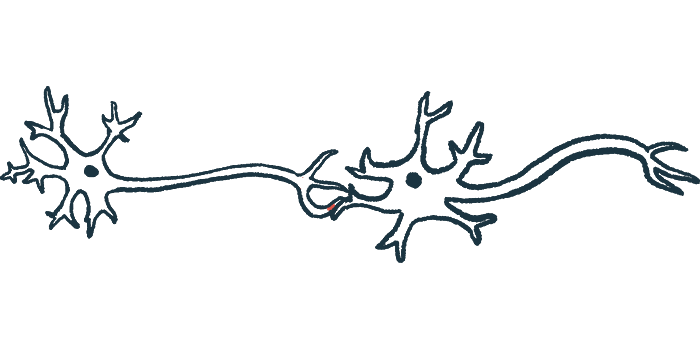
Parkinson’s disease is characterized by the progressive loss, in a midbrain region of the brain called the substantia nigra, of dopamine-producing neurons. Although there are three main groups of midbrain dopaminergic nerve cells (A8, A9, and A10), the A9 neurons have been found to be most affected in Parkinson’s.
A9 neurons are very large — possibly the largest cells in the human body — and express certain markers, such as ALDH1A1 and GIRK2.
“The cell is like the water supply system in a city, with a relatively small plant and hundreds of miles of water pipes going to each building,” Feng said in an analogy.
In the body, dopaminergic neurons in the substantia nigra are constantly active and firing action potentials, better known as nerve impulses. These pacemaking potentials are essential, as they ensure a consistent release of dopamine, which ultimately enables neurons to communicate and control movement.
“They depend on Ca2+ channels to maintain the pacemaking activities. Thus, the cells need to deal with a lot of stress from handling Ca2+ and dopamine,” Feng said. “These unique features of A9 DA [dopaminergic] neurons make them vulnerable. Lots of efforts are being directed at understanding these vulnerabilities, with the hope of finding a way to arrest or prevent their loss in Parkinson’s disease.”
One approach for replacing dopamine-producing neurons that has been investigated is the use of induced pluripotent stem cells, called iPSCs. These cells, which are typically derived from a certain type of skin cell, can be reprogrammed to develop into any other type of cell, including dopaminergic neurons.
Although previously established methods have worked well to differentiate human stem cells derived from embryos (hESCs) into midbrain dopaminergic neurons, these protocols were not as effective when used in iPSCs.
Now, Feng’s team came up with a new way of transforming human iPSCs into A9 dopaminergic neurons using small molecule compounds.
Human iPSCs were differentiated in three stages with varying chemicals to mimic what actually occurs during embryonic development. First, cells were developed into embryoid bodies, then into midbrain floor plate progenitors. In the last phase, they were differentiated into midbrain dopaminergic neurons. The timing, duration, and concentrations of the different chemicals were methodically optimized to direct the development of iPSCs all the way to A9 cells.
Researchers verified that their strategy allowed them to produce a large percentage of tyrosine hydroxylase-containing cells. Tyrosine hydroxylase is an enzyme that generates dopamine.
The cells that were produced were shown to express the A9 markers GIRK2 and ALDH1A1, and very little CALBINDIN, an A10 marker.
Functional studies confirmed that the lab-made A9 dopaminergic neurons had pacemaking abilities, which were dependent on Ca2+ channels. Additionally, as in typical dopaminergic neurons, the differentiated A9 cells also regulated dopamine release through D2 autoreceptors.
“Pacemaking is an important feature and vulnerability of A9 DA neurons. Now that we can generate A9 DA pacemakers from any patient, it is possible to use these neurons to screen for compounds that may protect their loss in [Parkinson’s disease],” Feng said. “It is also possible to test whether these cells are a better candidate for transplantation therapy.”
To see if A9 neurons could restore lost motor function, the team used a rat model of Parkinson’s. The rats were injected, directly into the brain, with 6-hydroxydopamine, a chemical that destroys dopamine-producing neurons. The animals were then transplanted with the lab-made A9 neurons.
Two movement tests were conducted: the apomorphine-induced rotations and latency to fall on a rotarod. Apomorphine induces circling behavior; a higher number of rotations means more extensive brain damage. In the rotarod test, a performance measure, the animal must remain upright on a slowly spinning horizontal rod.
By eight and 12 weeks after the procedure, rats transplanted with A9 neurons had a significantly lower number of apomorphine-induced rotations and better performance on the rotorod test than untransplanted rats.
“Our study showed that the human midbrain dopaminergic neurons that we differentiated from iPSCs had many important characteristics of A9 DA neurons. These results will stimulate efforts to replicate our findings and use the method to study the function and dysfunction of human A9 DA neurons,” the authors wrote.
“This exciting breakthrough is a critical step forward in efforts to better understand Parkinson’s disease and how to treat it,” said Allison Brashear, MD, vice president for health sciences at University at Buffalo.