New method may identify younger people at risk for Parkinson’s
Identifying toxic protein clumps in skin may enable early diagnosis, treatment
Written by |
A new method for detecting toxic protein clumps of alpha-synuclein in skin cells may help diagnose Parkinson’s disease up to two decades before motor symptoms appear, according to a recent study.
The novel technology combines super-resolution microscopy and advanced computational analysis to precisely map the protein clumps’ molecules and structures in skin samples.
“In this study we began to develop a research tool to enable diagnosis of Parkinson’s at a much earlier stage, when it is still treatable, and deterioration can be prevented,” Uri Ashery, PhD, a professor at Tel Aviv University and lead researcher on the study, said in a press release.
Their study, “A novel super-resolution microscopy platform for cutaneous alpha-synuclein detection in Parkinson’s disease,” was published in Frontiers in Molecular Neuroscience.
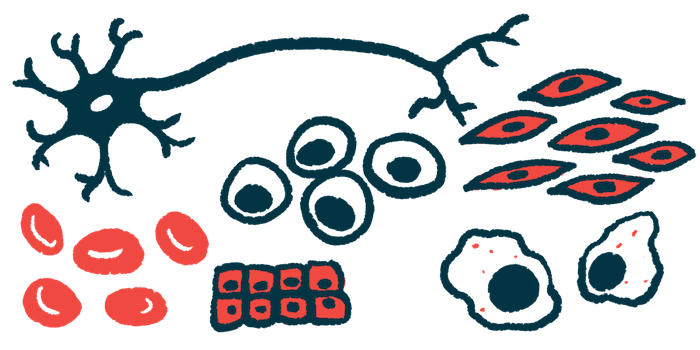
Parkinson’s disease is caused by the death of nerve cells (neurons) in the brain that are responsible for producing dopamine, a chemical messenger important for nerve cell communication. This death is often caused by the accumulation of toxic protein clumps, or aggregates, of alpha-synuclein.
Alpha-synuclein begins to form clumps about 15 years before symptoms show
Alpha-synuclein begins to form aggregates approximately 15 years before symptoms begin. Substantial cell death occurs in the five- to 10-year window before diagnosis, which is based mainly on clinical motor-related symptoms. By the time symptoms emerge, many dopamine-producing neurons will have died, limiting the efficacy of available treatments.
The researchers emphasized how critical it is to detect Parkinson’s before protein aggregates have caused such extensive cell death in the brain.
“If we can identify the process at an early stage, in people who are 30, 40, or 50 years old, we may be able to prevent further protein aggregation and cell death,” said Ofir Sade, a PhD student from Tel Aviv University who worked on the research.
Alpha-synuclein aggregates can form in other parts of the body outside of the brain, such as in the skin and digestive system.
In the current study, researchers looked at skin samples from seven Parkinson’s patients and seven people without the disease (controls) from three medical centers. They then processed the samples so they could identify these protein aggregates.
Samples were examined with a unique microscopy technique known as super-resolution microscopy, which allows researchers to capture images at nanoscale resolutions that can surpass the limits of traditional light microscopy.
The researchers then developed a user-friendly analysis platform, which combines multiple complex computer algorithms to analyze the generated images.
Skin samples from patients had more alpha-synuclein aggregates
Skin samples from those with Parkinson’s had a higher number of alpha-synuclein aggregates than those from healthy controls. These aggregates were also larger and denser in Parkinson’s patients.
Skin regions that had an overabundance of alpha-synuclein aggregates also showed signs of degeneration of nerve fiber tissue.
The Michael J. Fox Foundation for Parkinson’s Research is funding an expansion of these initial findings in a larger study. In the next phase, researchers will test the super-resolution microscopy and analysis platform in skin samples from 45 people with Parkinson’s disease and 45-90 healthy subjects.
The researchers plan to collaborate with computer scientists to correlate their findings under the microscope with motor and cognitive features of Parkinson’s in these larger scale studies.
Increasing the number of samples and developing machine learning algorithms in future studies will allow researchers to identify young individuals at risk for the disease.
“Our main target population are relatives of Parkinson’s patients who carry mutations that increase the risk for the disease,” Ashery said. “Specifically, we place emphasis on two mutations known to be widespread among Ashkenazi Jews.”
The researchers hope this “new molecular toolbox” could be used to quantitatively track disease progression, measure the efficacy of disease-modifying treatments, and serve as a measurable marker of disease that can be used to set objective thresholds for Parkinson’s patients recruited for clinical trials.
This microscopy and computational analysis method may be useful in the earlier diagnosis of other neurodegenerative diseases, such as Alzheimer’s disease, that are associated with protein aggregates in brain cells.
“Our method can be used to identify early signs and enable preventive treatment in young people at risk for developing Parkinson’s later on in their lives,” the researchers said in the press release.