New Method Captures Images of All Brain Areas Following Gene Therapy
A new method that allows imaging of all brain areas can help researchers monitor the success of gene therapy in the treatment of neurological diseases such as Parkinson’s.
The study, “A Novel Positron Emission Tomography Reporter Gene/Reporter Probe for the Central Nervous System,” was presented recently during the SNMMI 2018 Annual Meeting in Philadelphia, and published in the Journal of Nuclear Medicine.
Gene therapy is a therapeutic approach that has the potential, by replacing a defective gene copy with a healthy one, to be a one-time treatment that fixes, rather than treats, disease.
In neurological diseases – such as Parkinson’s disease or Alzheimer’s disease – gene therapy is often limited by the lack of an adequate imaging technique that can successfully help monitor the delivery and expression of the therapeutic gene directly into the brain.
While many reporter gene systems — a construct that tags genes with fluorescent probes and allows tracking within the body— have been developed for imaging gene therapies, current systems do not allow imaging all areas of the brain.
“It is challenging to find a reporter gene and imaging agent that can be used in all areas of the brain with a high signal-to-background ratio,” Thomas Haywood, PhD, department of radiology at Stanford University, said in a press release.
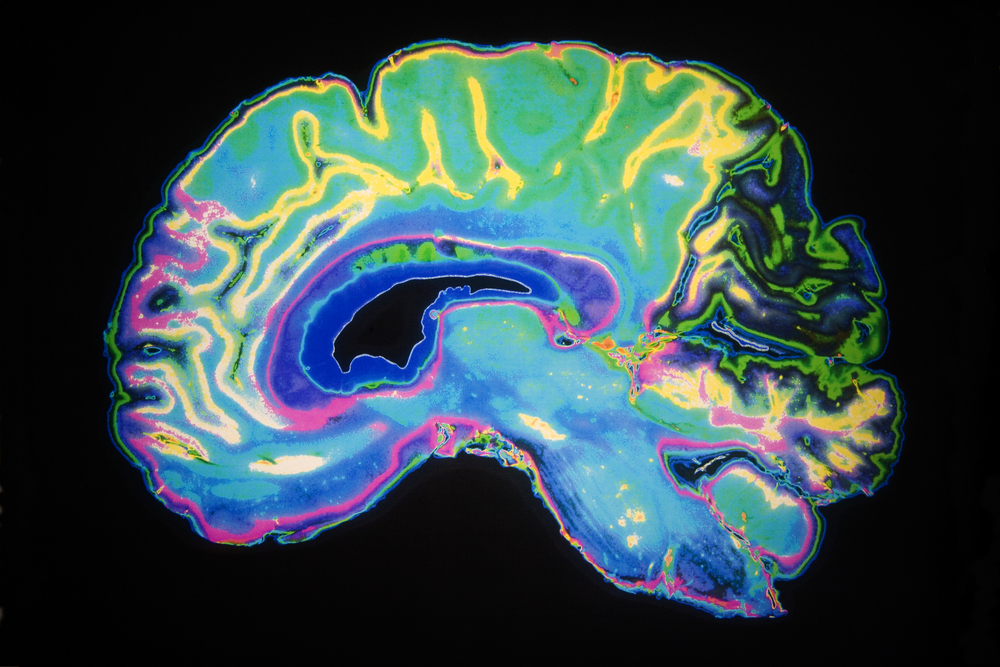
Researchers now have developed a new positron emission tomography (PET) reporter gene system that allows for monitoring of gene expression (the process by which information in a gene is synthesized to create a working product, like a protein) in all areas of the brain.
PET imaging uses small amounts of radioactive materials, called radiotracers, along with a special camera and computer to help evaluate organ and tissue functions.
The newly developed system allows researchers to monitor the level and location of gene expression in all areas of the brain in a non-invasive manner, helping physicians determine the likelihood of treatment success.
To test their new method, researchers infected mice brain cells with a viral vector containing the PKM2 gene. PKM2 was considered an ideal choice for a reporter gene because the protein it produces, pyruvate kinase M2, is not expressed at very high levels in the healthy brain. As such, it can be specifically monitored and traced in an experimental setting.
Animals then were imaged with the 18F-DASA-23 radiotracer over a period of two months to observe the increase in PKM2 expression over time. Importantly, this radiotracer is able to cross the blood brain barrier (BBB), a semi-permeable membrane that protects the brain from outside circulating blood.
“18F-DASA-23 is a novel radiotracer, or reporter probe, developed in the Gambhir lab at Stanford that is capable of crossing the blood–brain barrier and targeting the pyruvate kinase M2 protein in the central nervous system with minimal endogenous [normal] expression in the brain,” Haywood explained. “This allows us to monitor reporter gene expression and ultimately therapeutic gene expression for gene therapy in all regions of the brain.”
Results showed there was an increase in 18F-DASA-23 uptake, which correlated with the levels of PKM2 in the cells. This suggests that not only was PKM2 being expressed, but that the radiotracer was correctly detecting its expression in brain tissue.
“This encouraging data suggests PKM2 has the potential to be further developed into a PET reporter gene system for the imaging of gene therapy in the CNS [central nervous system],” the authors wrote.
“Having a reporter gene/reporter probe system that allows monitoring of all areas of the brain opens the door to more accurate and less invasive imaging of the brain and of gene therapies used to tackle diseases of the brain,” Haywood said.
A Phase 1 clinical trial is currently recruiting patients to test the 18F-DASA-23 radiotracer for the early detection of therapeutic response in patients with glioblastoma, a type of brain tumor that develops in certain brain cells called astrocytes.






