Dopamine neurons may be more diverse than thought
Cellular study of mice suggests 'new way of thinking about the brain'
Written by |
A specific subset of dopamine-producing nerve cells in the brain appear to respond to movement acceleration and correspond with the region where cell death is particularly pronounced in Parkinson’s disease, according to a recent study.
These neurons were responsive only to movement, and not to rewarding stimuli, which long had been considered a shared characteristic of all cells that release dopamine, a nerve-signaling chemical.
“Our results provide new potential research directions for different dopamine-related diseases, such as Parkinson’s disease,” the researchers wrote, adding that the study “warrants a reconsideration of the role of dopamine in motor and non-motor symptoms of Parkinson’s disease.”
The study, “Unique functional responses differentially map onto genetic subtypes of dopamine neurons,” was published in Nature Neuroscience.
Dopamine is best known for mediating the brain’s response to rewards, but also is involved in other behaviors such as responses to aversive stimuli and movement control.
Indeed, the progressive loss of dopamine-producing cells (dopaminergic neurons) in a brain region called the substantia nigra pars compacta (SNpc) is thought to underlie the hallmark motor symptoms of Parkinson’s disease.
“When people think about dopamine, they likely think about reward signals,” Daniel Dombeck, PhD, a professor at Northwestern University and one of the study’s senior authors, said in a press release.
“But when the dopamine neurons die, people have trouble with movement. That’s what happens with Parkinson’s disease, and it’s been a confusing problem for the field,” he said.
Still, it has been thought that all dopamine-producing cells in some way are involved in the reward process. Dombeck’s lab previously identified dopaminergic neurons that responded to movement in mice, but it didn’t really change that perception.
“Others continued to assume that all dopamine neurons were still reward neurons. Maybe some of them just had motor signals too,” Dombeck noted.
Three subtypes of dopamine neurons
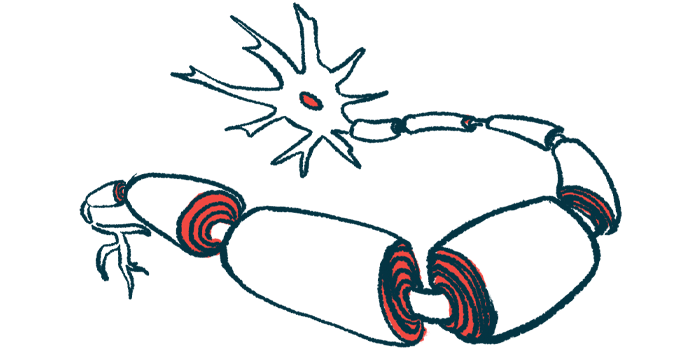
It’s been proposed that there are three subtypes of dopaminergic neurons, each distinguished by a defining genetic marker — Aldh1a1, Calb1, and Vglut2 — raising the possibility that different dopaminergic cell subtypes might mediate different dopamine-associated behaviors.
In their study, the scientists further examined the functions of these dopaminergic subtypes within the SNpc. Mice were engineered genetically so that each different cell type was tagged with a specific fluorescent marker. If those cells were active when the mouse was performing a particular behavior, they would glow.
Certain cells of the Aldh1a1 subtype glowed when the mice were moving. These movement-associated responses were observed in a subset of Aldh1a1-positive cells that project to another brain region called the striatum, which is crucially involved in movement control.
Notably, these cells sit “right where dopamine neurons first die in Parkinson’s disease,” Dombeck said. “That’s just another hint and clue that seems to suggest that there’s some genetic subtype that’s more susceptible to degradation over time as people age.”
Additional experiments identified that these movement-responsive cells were a distinct subset of Aldh1a1 dopamine cells also positive for a marker called Anxa1. While Aldh1a1-positive cells have been linked previously to Parkinson’s, it wasn’t known there potentially was a distinct subset of them that could be implicated.
Loss of dopamine signaling
“Motor deficits [in Parkinson’s] may not be due to an absolute dopamine deficiency but, rather, to a loss of dopamine signaling from specific pro-motor subtypes such as Anxa1+ neurons,” the researchers noted.
Notably, Anxa1 cells were found to respond specifically when mice were accelerating, whereas the Calb1, and Vglut2 cells preferentially signal when mice are slowing down.
“We’re wondering if it’s not just the loss of the motor-driving signal that’s leading to the disease — but the preservation of the anti-movement signal that’s active when animals decelerate,” Dombeck said.
“It could be this signal imbalance that strengthens the signal to stop moving. That might explain some of the symptoms. It’s not just that patients with Parkinson’s can’t move. It could also be that they are being driven to stop moving,” he added.
Calb1, and Vglut2 cells responded robustly to both rewarding and aversive stimuli, although their response profiles were different. On the other hand, Anxa1-positive cells did not respond at all to reward and actually decreased their activity in response to aversion.
“This goes against the dogma of what most people think these neurons should be doing,” said Rajeshwar Awatramani, PhD, a professor at Northwestern and one of the study’s senior authors.
“We’re still trying to figure out what this all means,” Awatramani said. “I would say this is a starting point. It’s a new way of thinking about the brain in Parkinson’s.”



