Molecular Link Found Between Parkinson’s and Skin Cancer
Written by |
Researchers have found a molecular link between Parkinson’s disease and melanoma, a type of skin cancer, in the form of protein clumps.
Their study results were presented at the spring meeting of the American Chemical Society this week.
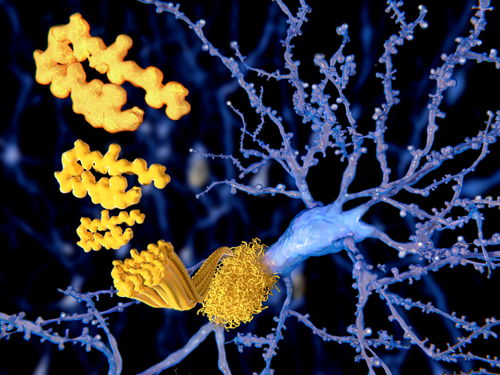
A hallmark of Parkinson’s disease is the buildup of alpha-synuclein protein clumps within brain cells. Alpha-synuclein aggregates are found mainly in dopamine-producing nerve cells, or neurons, where they appear to be involved in neuronal communication.
Despite the key role of protein aggregates in the brain and its contribution to the development and progression of Parkinson’s disease and other neurodegenerative disorders, such as Alzheimer’s disease, there is not much information about its presence and activity in other tissues.
“Several studies have shown that melanoma occurs two to six times more frequently in the Parkinson’s population than the healthy population,” Dexter Dean, PhD, postdoctoral fellow at the National Heart, Lung, and Blood Institute (NHLBI), said in a press release. “What’s more, the protein involved in Parkinson’s disease, α-synuclein [alpha-synuclein], is elevated in melanoma cells.”
Besides alpha-synuclein, another protein called premelanosomal protein, or Pmel, has been shown to aggregate and form fibril plaques, also known as amyloids.
“Most people know that amyloids are involved in diseases, such as Parkinson’s and Alzheimer’s, but it’s less well-known that some amyloids, like Pmel, actually serve a useful function,” said Jennifer Lee, PhD, Dean’s postdoctoral advisor at NHLBI. “In healthy melanocytes [skin cells], Pmel forms amyloid fibrils that act as scaffolds to store melanin.”
The researchers used imaging and protein detection techniques to understand where the two proteins — alpha-synuclein and Pmel — were located and whether they were interacting with each other.
“Because both α-synuclein [alpha-synuclein] and Pmel are expressed in melanoma cells, we wondered if these two amyloid proteins could interact, and whether this interaction could be relevant to the correlation between Parkinson’s disease and melanoma,” Lee added.
Results of the study show that both proteins are located in melanosomes — a cell organelle where pigment is produced, stored, and transported — of human melanoma cells.
The researchers then added preformed alpha-synuclein clumps to the amyloid-forming region of Pmel, known as the repeat domain. They observed that these protein fibrils stimulated Pmel to aggregate and form fibrils that it would not normally form on its own.
Additionally, when a soluble, or non-amyloid, form of alpha-synuclein was added to the Pmel repeat domain domain, it inhibited this protein’s ability to form aggregates.
“We now have preliminary data that suggest an amyloid from one protein can ‘seed’ or template amyloid from another, and in the soluble form, α-synuclein [alpha-synuclein] prevents Pmel aggregation,” Lee said. “Therefore, we think that both forms of α-synuclein [alpha-synuclein] could diminish melanin biosynthesis — the amyloid form by causing Pmel to form an unusual twisted structure, and the soluble form by stopping Pmel from aggregating like it should.”
Losing melanin in skin cells could be a contributing factor for the increased melanoma risk observed in Parkinson’s patients, according to the researchers.
“In future experiments, I’m really interested in understanding more about what α-synuclein [alpha-synuclein] is doing to promote melanoma proliferation, in addition to this interaction with Pmel,” Dean said.




