Long-Lived Gut Macrophages Key for Survival of Nerve Cells, Could Help Parkinson’s Research
Long-lived macrophages in the mouse gut are crucial for the survival of nerve cells in the gastrointestinal tract and for proper digestion, a finding that sheds new light not only on neurodegenerative conditions of the intestine, but also of the brain, researchers believe.
The study, “Self-Maintaining Gut Macrophages Are Essential for Intestinal Homeostasis,” was published in the journal Cell.
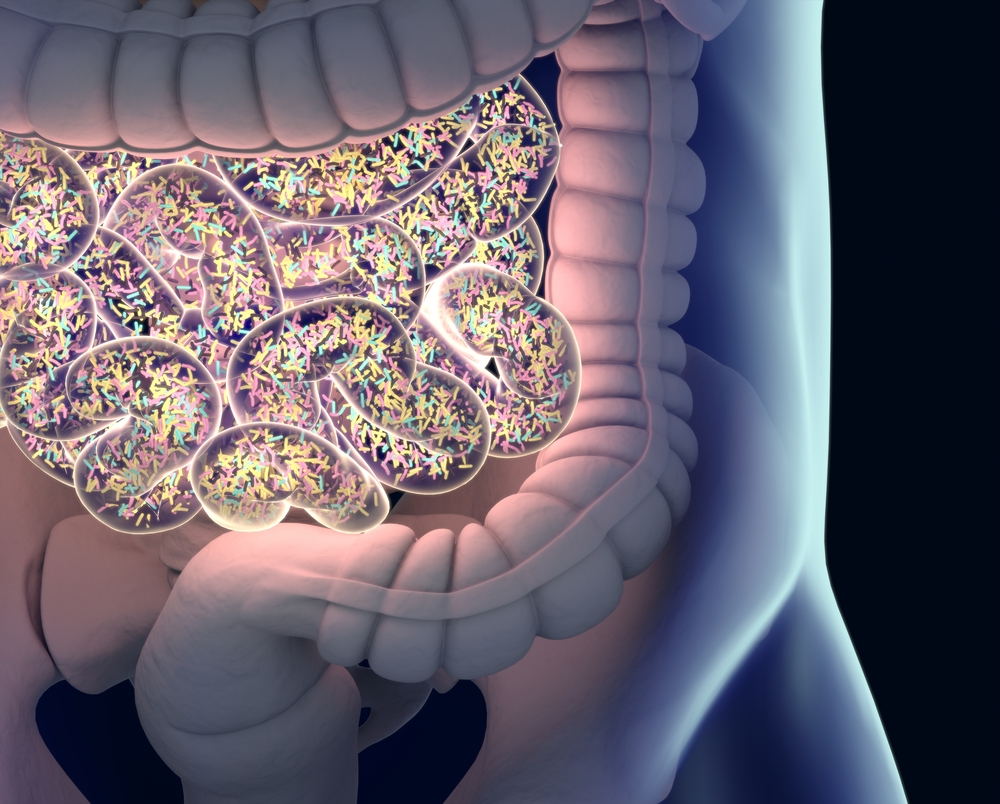
Macrophages are immune cells involved in the detection and destruction of bacteria and other harmful organisms, and they also participate in the initiation of inflammatory responses. This type of white blood cell also is a source of growth factors and support to different tissues, helping them function and develop properly. As such, macrophages play two opposing roles, of soldier and nourisher, at the same time.
Their correct functioning in the gut is critical, as these cells have to be able to differentiate between harmful bacteria, harmless bacteria and nutritional components. So-called gut-resident macrophages (gMacs) also contribute to the release of the anti-inflammatory molecule interleukin-10. They can be subdivided into various subpopulations with distinct characteristics.
Researchers believed that, after birth, intestinal macrophages were short-lived (approximately three weeks) and continuously replaced by bone marrow-derived monocytes (the largest of all white blood cells), which then would transform into macrophages.
Now, KU Leuven researchers have found this theory is not entirely correct. “We’ve discovered that a small part of the macrophages in mice is long-lived. We marked certain macrophages and found that they still functioned after at least eight months,” Guy Boeckxstaens, MD, PhD, the study’s senior author, said in a press release.
Specifically, researchers found that during embryonic life gMacs (self-maintaining macrophages) with a distinct pattern of gene expression colonize specific spots in the intestine, such as blood vessels and the myenteric plexus — the major source of nerve supply to the gut, connected to muscle cells. Gene expression is the process by which information in a gene is synthesized to create a working product, like a protein
After birth, these spots receive monocyte-derived gMacs, which implies that, similar to the heart and the lungs, the adult gut contains both embryonic, or long-lived, and monocyte-derived macrophages.
The scientists also found that long-lived macrophages support the organization and permeability of the gut’s lamina propria – a type of connective tissue – and muscularis externa, a muscle layer closely interacting with the intrinsic nervous system of the gastrointestinal tract, called enteric nervous system. Deleting the gMac population led to loss of enteric neurons, blood vessel leakage, and reduced intestinal motility.
“If the long-lived macrophages don’t do their job properly, already after a few days the mice suffer from digestive problems. This leads to constipation or even the complete degeneration of the nervous system in the stomach and intestine,” said Sebastiaan De Schepper, the study’s first author.
Overall, researchers believe that besides helping to better understand the diversity of this cell population, the results also “demonstrate the strategic role of self-maintaining [long-lived] macrophages in gut homeostasis and intestinal physiology.”
Investigators are now planning to study the role of these cells in disorders affecting nerve cells of the intestine, such as in obesity and diabetes.
“Moreover, the results can also be meaningful for brain research. In the brain, we have microglia, similar long-lived macrophages that play an important role in neurological conditions such as Alzheimer’s and Parkinson’s disease. Scientists currently believe that nerve cells in these patients die off because microglia do not provide sufficient care. Maybe one day research of the intestine can offer us a better understanding of these brain conditions,” Boeckxstaens said.






