Nasal Gel Enhances Levodopa Delivery to Brain in Preclinical Study
Written by |
Levodopa, a standard treatment for Parkinson’s disease, reached the brain faster when given as a gel into the nasal cavity than as an intravenous (into-the-vein) injection, a new mouse study shows.
The findings support the potential of intranasal administration as a way to reach the brain and bypass the breakdown of levodopa by the liver and gut — rendering it less available — when given orally, allowing patients to control their symptoms for longer.
The study, “Enhanced Delivery of Neuroactive Drugs via Nasal Delivery with a Self-Healing Supramolecular Gel,” was published in the journal Advanced Science.
The hallmark of Parkinson’s disease is the loss of dopaminergic neurons, those responsible for making the neurotransmitter dopamine, a chemical messenger that allows nerve cells to communicate and, among other functions, helps regulate movement.
Oral levodopa, or L-DOPA — a precursor to dopamine — is converted to dopamine once it reaches the brain and has long been one of the gold standards for Parkinson’s treatment.
However, over time the treatment becomes less effective, with patients requiring higher doses to ease symptoms. This is because metabolism of the substance is upregulated with prolonged exposure to levodopa and the compound is broken down by the liver and gut before reaching the brain. Eventually, in more severe cases, the therapy needs to be given intravenously.
“The current drug used for Parkinson’s Disease is effective to a point, but after a long period of use the body starts to breakdown the drug before it gets to the brain where it is most needed,” David Smith, PhD, professor at the University of York’s department of chemistry, and the study’s co-lead author said in a press release.
“This means increased dosage is necessary, and in later stages, sometimes, instead of tablets, the drug has to be injected,” he added.
Delivering therapeutics via the nasal cavity allows for a rapid absorption by the bloodstream, and is a direct way into the brain via the olfactory and trigeminal nerves, which transmit sensory information from the face to the brain.
In their study, researchers developed a gel loaded with levodopa. The gel first acts as a liquid when going in the nose but rapidly changes into a thin layer of gel. The gel adheres to nasal walls, providing a rapid release of the therapeutic agent.
“Investigations into nasal sprays have long been of interest as a more effective delivery because of its direct route to the brain via the nerves that service the nose, but the challenge here is to find a way of making it adhere to the nasal tissue long enough to release a good dosage of the drug,” Smith said.
Their system is based on a hydrogel consisting of a glutamine amide derivative and benzaldehyde, a substance used in perfumes and flavoring. Although benzaldehyde in high concentrations can cause nasal irritation, the hydrogel uses a lower concentration (0.115% weight/volume) than what is used in perfumes.
Characterization of its mechanical properties showed that the gel was extremely soft and therefore suited for nasal delivery.
“The results indicated that the gel gave the drug better adhesion inside the nose, which allowed for better levels of uptake into both the blood and brain,” Smith said.
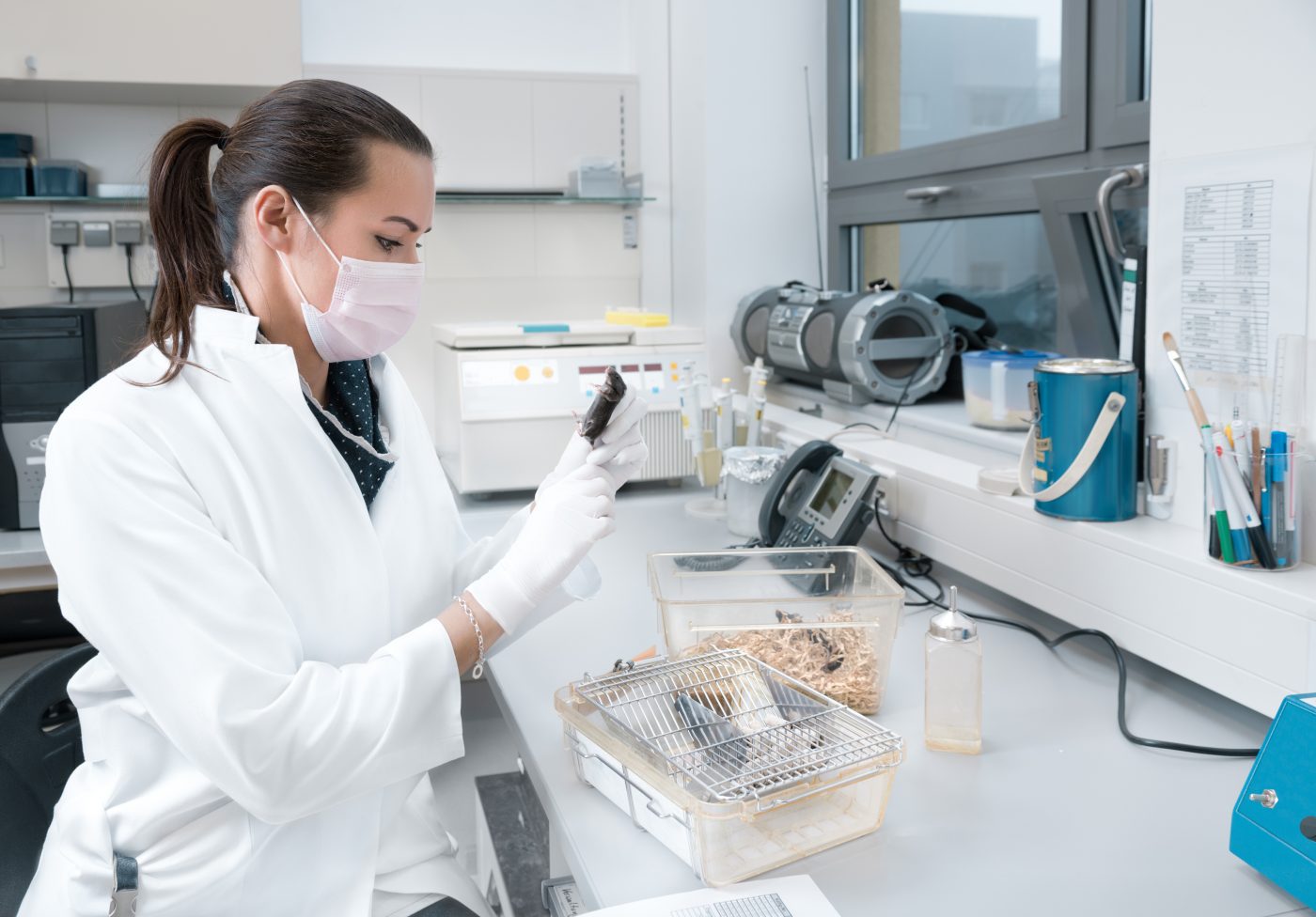
Next, the scientists used radiolabeled levodopa to analyze its distribution following intranasal administration into mice. They compared the distribution of levodopa when given as the hydrogel versus when given as a solution directly into the bloodstream.
Levodopa was detected in the brain, nasal cavities, and blood in both cases, but delivery into the brain was more efficient when using the hydrogel. Within 10 minutes after delivery, 27.55% of levodopa was found in the nasal cavity using the hydrogel, compared to 14.60% when given as a solution. Twenty minutes post-delivery, these values fell to 15.70% and 6.44%, respectively.
“Nasal delivery with our gel formulation therefore achieves 4.1 times more brain uptake of l-DOPA and 2.1 times more l-DOPA in the blood 10 min after administration than intravenous delivery of an equivalent dose,” the researchers wrote.
The researchers are now working on adapting their gel system into spray devices to be tested in clinical trials.
“Not only did the gel perform better than a simple solution, but the brain uptake was better than that achieved using intravenous injection of the drug,” said Khuloud Al-Jamal, PhD, professor and chair of drug delivery and nanomedicine at King’s College London, and co-lead author of the study.
“This suggests that nasal delivery of Parkinson’s drugs using this type of gel may have clinical relevance” she added.




