Delivery of stem cell therapy for Parkinson’s safe in primate trial
Transplant approach to delivering therapy feasible, study says
Written by |

A transplant approach used to deliver ANPD001, an investigational stem cell therapy for Parkinson’s disease, to the brain was found to be safe and feasible in non-human primates.
Data from these preclinical studies supported developer Aspen Neuroscience’s successful application to U.S. regulators seeking to launch a first-in-human study of the experimental treatment. The Phase 1/2a ASPIRO trial (NCT06344026) trial, enrolling by invitation only, is now testing ANPD001 in people with moderate to severe Parkinson’s disease.
“The study was an important step in our work to bring the promise of a cell-replacement therapy to people with Parkinson’s disease,” Andrés Bratt-Leal, PhD, co-founder and senior vice president of research and development at Aspen and one of the study’s authors, said in a company press release. “The results were instrumental in opening our first-in-human trial and informing how we deliver patients’ own cells.”
The Aspen-funded study, “Preclinical evaluation of transaxial intraputaminal trajectory for enhanced distribution of grafted cells in Parkinson’s disease,” was published in the Journal of Neurosurgery.
The symptoms of Parkinson’s disease are caused by the progressive loss of dopaminergic neurons, or nerve cells that produce the major brain signaling chemical dopamine. ANPD001 aims to replace these lost dopaminergic neurons as a way of slowing or stopping progression of the neurodegenerative disease.
Delivering stem cell therapy for Parkinson’s disease
The process involves collecting skin cells from a patient and reprogramming them in the lab to return to a stem-cell like state. Stem cells are a type of cell that can give rise to virtually all other mature cell types in the body, which means they can be leveraged to make more of whatever cells are lacking.
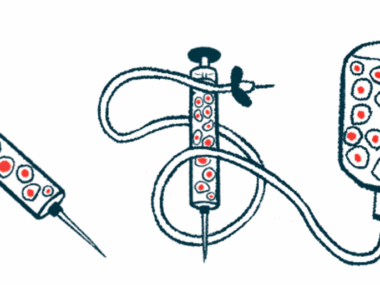
In this case, these so-called induced pluripotent stem cells, or iPSCs, are treated with chemicals in the lab that prompt them to turn into dopaminergic neuron precursor cells, which are then returned to the patient via a surgical transplant procedure.
The procedure specifically intends to deliver the therapy to the putamen, a brain region particularly affected in Parkinson’s, where the precursor cells can repopulate the area with functional dopaminergic neurons.
To ensure precise delivery, ANPD001 is given via an MRI-guided approach called the ClearPoint Navigation System. A surgeon will insert a thin tube called a cannula into the brain, while being provided real-time navigation instructions to reach the right part of the putamen. The cells are then infused, a few microliters at a time, through that tube.
The study was designed to test the feasibility of the transplant approach in non-human primates.
The research was led by Marina Emborg, MD, PhD, a professor at the University of Wisconsin-Madison and the study’s first author. Previous work from Emborg showed that a similar transplant approach, but using cells derived from the monkeys themselves, relieved motor and depression symptoms in a non-human primate model of Parkinson’s.
Now, the scientists administered Aspen’s human-derived cells to six primates. The cells were injected into the putamen on both sides of the brain, with a higher dose given on one side. Three animals underwent the surgical procedure without cell delivery.
The cannulas were inserted through the back of the skull, an approach intended to allow surgeons to achieve maximum cell distribution with fewer cannula insertions.
“The core idea is to decrease the risk of infection, the trauma, the surgical time the patient spends under anesthesia,” Emborg said in a university press release. “The fewer tracks you have to follow through the brain, the better for all of that.”
Results showed that the optimized technique was successful, and all animals survived the procedure. Some cases of mild brain swelling and reduced vision were managed with mannitol, a medication that can lower pressure in the brain and eyes, and an optimized infusion of fluids during surgery.
Tissue analyses showed that the transplanted cells took hold in the putamen for all but one of the treated animals, with more dopaminergic neurons found on the side that received a higher dose.
Any observed damage in brain tissue was limited and consistent with the surgery or injection procedure, or inflammation related to the cannula track.
“Our results were all so exciting,” Emborg said. “And then, when I saw they had been able to begin with a human patient this spring, I just had tears in my eyes.”
The open-label ASPIRO trial is testing the long-term safety and efficacy of escalating doses of ANPD001 in up to nine people with moderate or severe Parkinson’s, ages 50-70. The first transplant was performed earlier this year.
While the main goal is safety and tolerability, secondary efficacy outcomes will look at how well the therapy controls motor symptoms and improves life quality for Parkinson’s patients. Researchers will also examine how long the transplanted cells survive in the brain.