CuPiD Smartphone App May Prevent Dangerous Freezing of Gait in Parkinson’s Patients
Written by |

Many late-stage Parkinson’s disease patients have a high risk of suffering dangerous, sometimes fatal, falls. A major reason for increased propensity for falling is the disabling Parkinson’s symptom referred to as “Freezing of Gait” (FoG) — brief episodes of inability to step forward typically occurring during initiation of a step or when turning while walking.
Patients who experience frequent FoG often lose their independence, directly exacerbating an already degenerating quality of life. Absent effective pharmacological therapies for FoG, technology-based solutions to alleviate the symptom and prolong patients’ ability to live independently are desperately being sought.
CuPiD is a research and development project three years in the making by an eight-member European Union-funded consortium led by the University of Bologna in Italy, and is an FP7 ICT Collaborative Project including researchers at Israel’s Tel Aviv University (TAU). The CuPiD project’s objective is to provide personalized rehabilitation for patients with Parkinson’s disease who experience FoG and/or other gait disturbances. Through the CuPiD project the consortium will design, develop and test in the field an overall service, based on personal health system technology, for at home rehabilitation and training of major motor impairments caused by Parkinson’s disease.
Parkinsons disease (PD), a neurodegenerative disorder of unknown cause, particularly affects areas of the brain involved in movement control. Because PD is a neurological disorder with progressive disability over time, merits of rehabilitation have been questioned. However, over the past two decades, there has been a shift of attitudes due to evidence that the brain affected by PD may be capable of plasticity, and brain activity patterns may be altered with appropriate intensive training. The CuPiD team notes that research studies confirm the value of motor learning in PD, as well as showing improvements as a result of training.
“FoG is a leading cause of disability in patients with Parkinson’s disease,” says Prof. Jeffrey Hausdorff of TAU’s Sackler Faculty of Medicine and the Center for Movement, Cognition, and Mobility at Tel Aviv Sourasky Medical Center (TASMC). Prof. Hausdorff is the lead investigator on the Israeli team. “It often occurs during ‘walking transitions’ associated with turning, starting, stopping, and moving in open spaces. It can also occur when people approach narrow spaces, such as doors or elevators, and in crowded places. Recognizing such situations is a very powerful key for prevention and this is one of the features of this program.”
Prof. Hausdorff and his team at Tel Aviv Medical Center conducted a pilot study on 40 subjects: 20 patients with Parkinson’s disease who used the CuPiD app and 20 patients who carried out conventional exercises and did not use the app. The results are promising and the investigators are currently exploring the possibility of a larger follow-up study to further demonstrate the app’s efficacy.
 Dr. Anat Mirelman, also of TAU and TASMC, co-directed the pilot study. She explains that FoG episodes resemble a “short circuit” in the brain, rendering it unable to generate the appropriate stepping pattern, often leaving the patient in an untenable and frustrating situation. The app is designed to circumvent that difficulty.
Dr. Anat Mirelman, also of TAU and TASMC, co-directed the pilot study. She explains that FoG episodes resemble a “short circuit” in the brain, rendering it unable to generate the appropriate stepping pattern, often leaving the patient in an untenable and frustrating situation. The app is designed to circumvent that difficulty.
“There are two modes to the app,” says Dr. Mirelman. “The first improves the overall gait pattern — ‘keep it up, you are walking well,’ says a virtual physical therapist — and the positive feedback while walking actually helps the patient emotionally as well as functionally. If the gait pattern needs adjustments, the app will let the user know. The second mode helps patients avoid and free themselves of FoG if they are already stuck. We believe, and we have already seen in clinical trials here at the hospital, that this has the potential to improve the quality of life for these patients quite dramatically.”
“FoG reduces patients’ independence. Patients become afraid of walking by themselves and this leads to self-imposed restrictions in mobility,” Dr. Mirelman observes, “their feet get stuck to the ground, their bodies lunge forward it’s very frightening. People often end up in wheelchairs, and this is a vicious cycle, as it places more reliance on the assisted-living infrastructure.”
“The program now integrates the expertise of a patient’s physical therapist, who establishes what is considered a patient’s ‘normal’ or ‘strong’ walking pattern,” says Prof. Hausdorff. “It’s unobtrusive and has the potential to reduce dependence on Parkinson’s medication that has detrimental side effects. How much or how often the app is used depends on how advanced the disease is, but since the system is so small and non-invasive, it can be used just about anywhere. It’s exciting to think of the potential of long-term use.”
The CuPiD project will develop innovative rehabilitation based on new technology, the patient’s needs, and the principles of motor learning in PD. CuPiD will contribute to the challenge of engaging patients with a chronic neurodegenerative disease in intensive exercise for a considerable length of time.
The rehabilitation service being developed in CuPiD is intended for delivery outside hospitals and care centres. It will be designed to be ubiquitous, so that it can be easily delivered at patients’ homes, or in some specific cases (e.g. gait training, which needs adequate space for performing long-distance walking) outdoors or in their preferred environment.
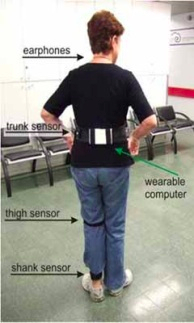 CuPiD will provide a ground-breaking home-based personalized rehabilitation tool for patients with Parkinson’s disease in the form of a smartphone app that harnesses wearable sensors, audio biofeedback, and external cueing to provide technology-driven personalized rehabilitation exercises for people with Parkinson’s disease at home, with the intense motivational training custom-tailored to each individual patient. Data can be monitored remotely by medical professionals, who provide quality care while enhancing patient compliance. CuPiD will monitor and record remotely a patient’s activity in training and clinicians will be able to supervise their progression, change the training to fit an individuals needs and assess problems that occur using a computer interface.
CuPiD will provide a ground-breaking home-based personalized rehabilitation tool for patients with Parkinson’s disease in the form of a smartphone app that harnesses wearable sensors, audio biofeedback, and external cueing to provide technology-driven personalized rehabilitation exercises for people with Parkinson’s disease at home, with the intense motivational training custom-tailored to each individual patient. Data can be monitored remotely by medical professionals, who provide quality care while enhancing patient compliance. CuPiD will monitor and record remotely a patient’s activity in training and clinicians will be able to supervise their progression, change the training to fit an individuals needs and assess problems that occur using a computer interface.
The large amount of data gathered will allow research on the basic mechanisms of training in people with PD and the correlation between context (i.e. medication intake, stress, location, attention level) and motor performance. New algorithms for feedback will be developed and validated. CuPiD provides an innovative Personal Health System with on-board processing enabling multi-modal feedback and multi-faceted training. CuPiD will guarantee usability and personalization of rehabilitation, empowering the end-user to self-manage his/her training at-home, and will contribute to the use of standardisation in health IT.
CuPiD’s three services include:
Exergaming which will provide audio, visual and tactile feedback while the patients train using different simulations. This training requires integration of cognitive (attention, decision making) and motor function in a motivating and engaging environment.
Provision of external cues to avert freezing of gait (FOG) and training of its prevention. (Can include outdoor usage)
Biofeedback device for training of daily activities; the device will be portable and able to provide audio, visual and tactile feedback for the training of motor/cognitive functions. (can be used outdoors)
CuPiD will develop and validate a personal health service with: Exergaming. This is a powerful tool for repetitive practice of motor function, providing feedback about performance and motivation for patients.
Wearable components. These will be connected to a exergaming simulation whose feedback will enhance training.
CuPiD will offer a device which will realize freezing of gait rehabilitation by predicting onset of a freezing episode and provide feedback shortly before the freeze. This can be used by a trained patient to consciously balance his/her body weight, thus providing assistance in case of freeze. Through repeated occurrences, patients will internalize this feedback process, learning to overcome and manage freezing episodes.
In the first half of the project, sensor configurations will be tested to increase specific applications knowledge. Tests will include wearable sensors, motor-task identification, efficacy of feedback restitution, real-time biofeedback, interface development and exergaming based simulation.
The second half of the project consists of a large validation campaign to allow accurate evaluation of the services in terms of:i) feasibility; ii) integration with healthcare institutions; iii) efficacy of intervention; iv) satisfaction of all users.
The CuPiD project will include 2 long term trials each lasting approximately 10 weeks and consisting of 30 Parkinsons disease patients. CuPiiDs Israeli and Belgian clinical partners will be responsible for this area of the project.
The CuPiD app just completed its pilot run and is being fine-tuned for more widespread use. It utilizes small sensors placed on a patients’ shoes that measure a persons gait in “real-time.” If certain deviations from a pre-set norm emerge, an audio message alerts the patient to change his or her walking pattern immediately to avoid a dangerous situation.
Sources:
The CuPiD project
Tel Aviv University (TAU)
Image Credits
The CuPiD project
Tel Aviv University (TAU)


