Changes in Protein Structure May Act as Parkinson’s Biomarkers
Differences seen in 76 proteins in patients' cerebrospinal fluid could aid diagnosis

Changes in the structure of 76 proteins in the cerebrospinal fluid (CSF) of people with Parkinson’s disease were seen when compared with those of healthy individuals, a study reported.
Its researchers believe their work is the first to look at protein structure — rather than abundance — to identify potential new biomarkers for diagnosing Parkinson’s.
“From what we’ve seen so far, they’re actually a very strong indicator for the disease. So I’m confident that this idea of structural biomarkers will bear out,” Natalie de Souza, PhD, a study author and professor of molecular systems biology at ETZ Zurich, said in a university press release. De Souza is a senior scientist in the lab of Paola Picotti, PhD, the study’s senior author.
The study, “Global, in situ analysis of the structural proteome in individuals with Parkinson’s disease to identify a new class of biomarker,” was published in the journal Nature Structural & Molecular Biology.
Study aiming for more accurate biomarkers in diagnosing Parkinson’s
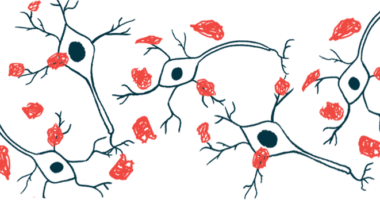
Proteins are complex molecules that fold into unique three-dimensional shapes or structures that allow them to specifically interact with other molecules to exert their function. As such, alterations in protein structure can lead to changes in how they work.
Hypothesizing that most molecular events affecting protein function likely affect their structure, a research team led by ETH Zurich scientists evaluated whether proteins in Parkinson’s patients showed a distinct structure to people without any disease.
Their goal was to determine whether abnormally structured proteins represented a new disease biomarker.
The researchers analyzed the CSF, the liquid surrounding the brain and spinal cord, of 51 Parkinson’s patients (mean age of 62.9) at early disease stages (mean duration, 5.8 years) and 52 healthy people (mean age of 63.1) as a control group.
To profile the proteome, or entire set of proteins, in the CSF, they used a technique called limited proteolysis–mass spectrometry (LiP–MS), which can identify proteins and detect specific changes in their shape. Conventional proteome methods typically identify proteins and measure their levels, but not their structural changes.
Over 2,100 proteins and more than 48,000 peptides — short chains of amino acids, the building blocks of proteins, and essential on their own for many body processes — were analyzed. Of these, 859 proteins and 7,144 peptides underwent further evaluation. Structural changes were evident in 88 peptides corresponding to 76 proteins in Parkinson’s patients relative to healthy controls, the researchers reported.
Importantly, proteins with altered shape were linked to pathways known to be dysregulated in Parkinson’s disease.
All but one of the 88 peptides showing structural changes in patients “were classified as non-variable in our analysis of healthy CSF and are therefore not likely to be confounded by background variability,” the researchers wrote, meaning these changes are likely to be seen across people with Parkinson’s.
Researchers then assessed whether structurally abnormal proteins and peptides in the CSF might be found in patients’ brains, using post-mortem tissue samples from 10 women: five with Parkinson’s and five age-matched women without the disease.
In total, 27 of the 76 proteins and 11 of the 88 peptides with a structural change in the CSF were also detected in the brain samples. Most importantly, 16 of these proteins and eight peptides showed structural alterations in both the brain and CSF of patients relative to controls.
15 proteins, all tied to Parkinson’s, show changes in patients’ CSF and brain tissue
More detailed analysis revealed that 15 of these 16 proteins were previously linked with Parkinson’s, including proteins that regulate neurotransmission like that mediated by dopamine, the chemical messenger essential for muscle control that is lost in Parkinson’s. Neurotransmission is a form of chemical communication between nerve cells, taking place at specialized sites termed synapses.
Variations in the genes coding for two CSF proteins — COL3A1 and PAM — and three brain proteins — AAK1, CYRIB, and APOE — were previously identified as genetic risk factors for Parkinson’s.
“We observe structural variation in various classes of proteins, including enzymes and proteins involved in synapse organization and function, that are strongly linked to PD [Parkinson’s disease],” the scientists wrote.
The researchers then assessed whether a combination of structurally abnormal peptides in the CSF could serve as biomarkers for distinguishing people with Parkinson’s from healthy individuals.
Overall, results showed that this model was superior to a model based on protein abundance at discriminating Parkinson’s patients. The area under the curve (AUC) — a measure of how good a biomarker is, with one representing a perfect score — showed that this structure-based model had a score of 0.752 compared with 0.673 for a model based on protein levels.
Finally, their model’s performance was compared to a model based on CSF levels of alpha-synuclein — “the best currently available potential [Parkinson’s] biomarker,” the researchers wrote.
Alpha-synuclein is a protein that forms toxic clumps in the brain of Parkinson’s patients and is the main component of the disorder’s hallmark Lewy bodies.
The researchers’ model “slightly outperformed” the alpha-synuclein-based model, which showed an AUC score of 0.733, they reported. But it did not outperform models based on the levels of the toxic form of alpha-synuclein (AUC of 0.799) or the ratio between the toxic form and total alpha-synuclein (AUC of 0.838).
“Overall, our data provide strong support for the hypothesis that protein structural changes provide more information about the PD state than protein abundance information,” the researchers wrote.
They noted, however, that a model combining LiP–MS (limited proteolysis–mass spectrometry) and alpha-synuclein quantification may help to more accurately identify Parkinson’s patients.
“Our results suggest that global structural analyses of the CSF proteome may identify PD biomarkers complementary to existing [alpha-synuclein-based] measures, which may be combined with these measures to improve power to classify individuals with the disease,” the team wrote.
In the future, the researchers aim to validate their findings in a larger Parkinson’s group and optimize the LiP-MS method to increase its sensitivity in detecting Parkinson’s.
They also want to determine whether their method can help in distinguishing Parkinson’s subtypes and making more accurate predictions regarding disease progression, as well as testing the biomarkers’ specificity for Parkinson’s by analyzing their performance in other neurodegenerative diseases, such as Alzheimer’s.
Strategies based on antibodies to recognize and distinguish normal and abnormal protein structures would be more a feasible tool for everyday clinical use than mass spectrometers, the researchers believe.
“Making regular use of mass spectrometers in a clinical setting is in principle possible but would be a big challenge” De Souza said.