Breathing low oxygen air could be new model for treating Parkinson’s
In mice, novel strategy found to ease or reverse motor symptoms
Written by |

Continuous exposure to low-oxygen air halted neurodegeneration and eased or reversed motor symptoms in a mouse model of Parkinson’s disease, a study reports.
“The results raise the possibility of an entirely new paradigm for addressing Parkinson’s,” Fumito Ichinose, MD, PhD, senior coauthor of the study, said in a news story from the Broad Institute in Massachusetts, where some of the research team are based.
It is too early to translate these results to humans, and the researchers cautioned against unsupervised breathing of low-oxygen air. However, these findings suggest possibilities for future Parkinson’s treatments, according to the team of U.S. researchers.
The scientists noted that “unfortunately, no therapies currently exist to halt or slow the progression of neurodegeneration in patients with PD [Parkinson’s disease].”
This study “reports that breathing [low-oyxgen air] not only prevents but also reverses motor deficits in a PD mouse model,” the team wrote.
Titled “Hypoxia ameliorates neurodegeneration and movement disorder in a mouse model of Parkinson’s disease,” the study was published in the journal Nature Neuroscience.
Parkinson’s is caused by the death of nerve cells, called dopaminergic neurons, that produce the key chemical signaling molecule dopamine. Because these cells are important in pathways involving movement, their loss can lead to tremor and other motor symptoms.
However, the underlying triggers of dopaminergic neuron death remain unclear. Evidence suggests that toxic clumps of the protein alpha-synuclein may contribute to this neurodegeneration.
These clumps, or aggregates, may have a particularly detrimental effect on mitochondria, structures within cells that help turn oxygen into usable energy, research has shown. When mitochondria stop working properly, levels of oxygen can rise to potentially damaging levels.
Breathing low-oxygen air induces state known as hypoxia
Breathing low-oxygen air to induce a state called hypoxia may prevent this buildup, according to the research team. Anecdotally, some people with Parkinson’s describe their symptoms easing at high altitudes, where oxygen content in the air is lower. Long-term smokers also have a lower risk of developing Parkinson’s, which some scientists have theorized is partially related to slowed oxygen delivery.
“Based on this evidence, we became very interested in the effect of hypoxia on Parkinson’s disease,” Ichinose said. Adding to this, previous work has suggested a potential protective effect of hypoxia in other neurodegenerative disorders, such as Friedreich’s ataxia and multiple sclerosis.
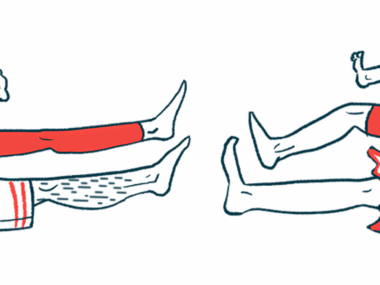
To test the impacts of hypoxia, the team used a mouse model of Parkinson’s. The animals received injections of alpha-synuclein, which, if left untreated, leads to Parkinson’s-like neurodegeneration and motor symptoms.
One group of mice stayed at normal oxygen levels — 21% oxygen, also called normoxia. The other lived in hypoxic conditions, at 11% oxygen, similar to the oxygen level at an altitude of about 16,000 feet. The hypoxic conditions were started immediately after injection.
While both animal groups developed alpha-synuclein aggregates, they only resulted in significant dopaminergic neuron loss for mice breathing normal air.
As such, the researchers determined that “hypoxia does not prevent the formation of [alpha-synuclein] aggregates. Rather, hypoxia confers neuroprotection in the face of these aggregates.”
Researchers: ‘Too much oxygen in the brain turns out to be toxic’
Supporting this, the hypoxia group performed better on several tests of motor function three months after their injection with alpha-synuclein. In fact, the results were similar to those of control animals. Normoxia animals, on the other hand, showed significant reductions in motor abilities at this time point. The relative benefits of hypoxic conditions on some motor tests remained for at least 10 months, the data showed.
A separate group of animals received alpha-synuclein injections, then stayed at normal oxygen levels for six weeks. At this point, there were no signs of significant dopaminergic neuron damage, although motor abilities declined, according to the researchers.
The fact that we actually saw some reversal of neurological damage is really exciting. … It tells us that there is a window during which some neurons [nerve cells] are dysfunctional but not yet dead — and that we can restore their function if we intervene early enough.
After this period, some of the mice transitioned to hypoxic conditions for another six weeks. In these mice, but not those who remained in normoxia, motor performance significantly improved. The animals that continued to breathe normal air also showed significant cell death, while mice in low-oxygen conditions did not, indicating a slowing or halting of neurodegeneration.
“The fact that we actually saw some reversal of neurological damage is really exciting,” said Vamsi Mootha, MD, the study’s co-senior author. “It tells us that there is a window during which some neurons are dysfunctional but not yet dead — and that we can restore their function if we intervene early enough.”
Altogether, the study’s findings support the idea that “too much oxygen in the brain turns out to be toxic,” Mootha said. “By reducing the overall oxygen supply, we’re cutting off the fuel for that damage.”
Future research needed to potentially translate findings to humans
One potential mechanism supporting this process could be hypoxia-related changes that gene cells are expressing. The team saw significant differences in expression, or activation, of certain genes, including some related to adaptation to hypoxic conditions.
Future research will need to address possible damaging effects of sustained hypoxia, according to the team. It is also unclear how hypoxia therapy could safely translate humans. Intermittent low-oxygen exposure and pharmaceutical options that mimic conditions of hypoxia are potential future avenues for exploration.
Researchers could also investigate the impacts of hypoxia on other neurodegenerative diseases.
“It may not be a treatment for all types of neurodegeneration, but it’s a powerful concept — one that might shift how we think about treating some of these diseases,” Mootha said.