Bach1 Protein Blocker Seen to Protect Nerve Cells, Ease Symptoms in Mice
Written by |
A new, potent inhibitor of the Bach1 protein — whose levels are elevated in brain tissue of Parkinson’s disease patients — showed neuroprotective effects in lab tests and lessened symptoms in a mouse model of acute Parkinson’s, a study found.
Most importantly, the inhibitor had therapeutic potential when administered either before disease onset or after symptoms were already evident in the mice.
“This is the first evidence that Bach1 is dysregulated in Parkinson’s disease,” Bobby Thomas, PhD, a professor of pediatrics at the Medical University of South Carolina (MUSC) and the study’s lead author, said in a press release. MUSC scientists, in collaboration with vTv Therapeutics, are developing the potential treatment.
Parkinson’s disease is characterized by the buildup of the alpha-synuclein protein in the brain, resulting in the death of nerve cells, or neurons, that produce the neurotransmitter dopamine — a chemical messenger essential for muscle control.
This accumulation of alpha-synuclein induces oxidative stress — an imbalance between the production of harmful free radicals and the ability of cells to detoxify — which contributes to cell damage and death.
Current therapies work to lessen symptoms but fail to tackle the causes of nerve cell death, the MUSC researchers noted. A treatment’s efficacy also often declines with time.
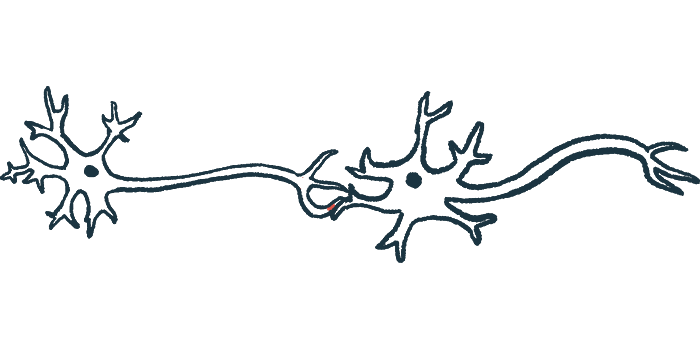
Nerve cells have mechanisms to protect against oxidative stress, including the activation of two key proteins, called Nrf2 and Bach1. Nrf2 regulates the expression (activity) of over 250 genes in an orchestrated effort to protect cells from oxidative stress, while Bach1 has an opposite role: it actually prevents these genes from being activated.
In their study “Bach1 derepression is neuroprotective in a mouse model of Parkinson’s disease,” published in the journal Proceedings of the National Academy of Sciences, researchers analyzed post-mortem brain tissue samples from Parkinson’s patients and found that the levels of Bach1 were abnormally high. Elevated levels were also observed in preclinical work in brain tissue samples from animal models of the disease.
These initial observations pointed to a potential role of Bach1 in Parkinson’s progression. To confirm its role, the researchers depleted the Bach1 gene in a mouse model of Parkinson’s, in which the disease was induced by exposing the animals to the MPTP neurotoxin.
Mice without Bach1 were protected against Parkinson’s disease induced by MPTP.
To understand how the loss of Bach1 protected neurons from oxidative stress, the researchers analyzed the genome of the brain in mice that had been depleted for Bach1.
As previously reported, they saw that Bach1 repressed the expression of Nrf2 protective genes and also regulated the activity of additional genes outside of the Nrf2 protein’s control.
“What we found was that Bach1 not only represses the expression of protective genes that are under the control of Nrf2, but it also regulates the expression of many other genes not directly regulated by Nrf2,” Thomas said. “So there are additional advantages to inhibiting Bach1 besides just activating Nrf2. Ideally you would want a drug that inhibits Bach1 and also activates Nrf2.”
Overall, “the functional genomics analysis of gene expression data from Bach1 [depleted mice] revealed activation of various pathways that are involved in neuroprotection, neutralizing oxidative stress, and balancing cellular inflammatory environment,” the researchers wrote.
Thomas and colleagues then teamed up with scientists at vTv Therapeutics, based in North Carolina, to develop Bach1 inhibitors.
Among the several candidates they tested, one called HPPE showed strong potential as a Bach1 blocker.
HPPE eased disease symptoms when administered to the MPTP mouse model of Parkinson’s. And, notably, the inhibitor’s potential was maintained when given either before MPTP — prior to disease onset — or after the animals started to show symptoms.
In lab tests, HPPE worked to protect cells from oxidative stress. Further analyses showed that HPPE was a potent activator of Nrf2 while it turned off pro-inflammatory genes.
Notably, HPPE was better than Tecfidera (dimethyl fumarate), an NRF2 activator currently approved to treat multiple sclerosis, and may carry fewer side effects.
Current NRF2 activators work as electrophiles, meaning they form a permanent bond and modify their target protein. This can lead to toxic buildups inside cells or cause the activation of the immune system, leading to several side effects.
“The most interesting aspect of the study is that the Bach1 inhibitor is a non-electrophile, so it doesn’t work like the FDA-approved Nrf2 activators,” Thomas said. “As a result of this difference, hopefully, HPPE will not demonstrate as many side effects.”
The “disruption of Bach1 and the simultaneous activation of Nrf2 clearly provide a strong basis for using HPPE as a potential therapeutic in [Parkinson’s disease],” the team wrote.
But while these data support HPPE as a potential treatment, further research is necessary to understand its effects with longer-term use, as well as its effectiveness in other mouse models of Parkinson’s, the researchers noted.
While the MPTP mouse is a model for acute disease — a disease with a rapid onset and/or short duration — scientists need to assess HPPE in models of chronic Parkinson’s, as well as its potential in other neurological diseases characterized by inflammatory response and mitochondria dysfunction. (Mitochondria are a cell’s powerhouse, or the producers of energy within cells.)
“This pathway may be beneficial whenever you have impairments in anti-inflammatory pathways or mitochondrial dysfunctions,” Thomas said. “I think any disease that has these kinds of etiologies [causes] would benefit from modulating this pathway.”