Autoantibodies May Link Ulcer Bacteria, Parkinson’s Disease
Written by |
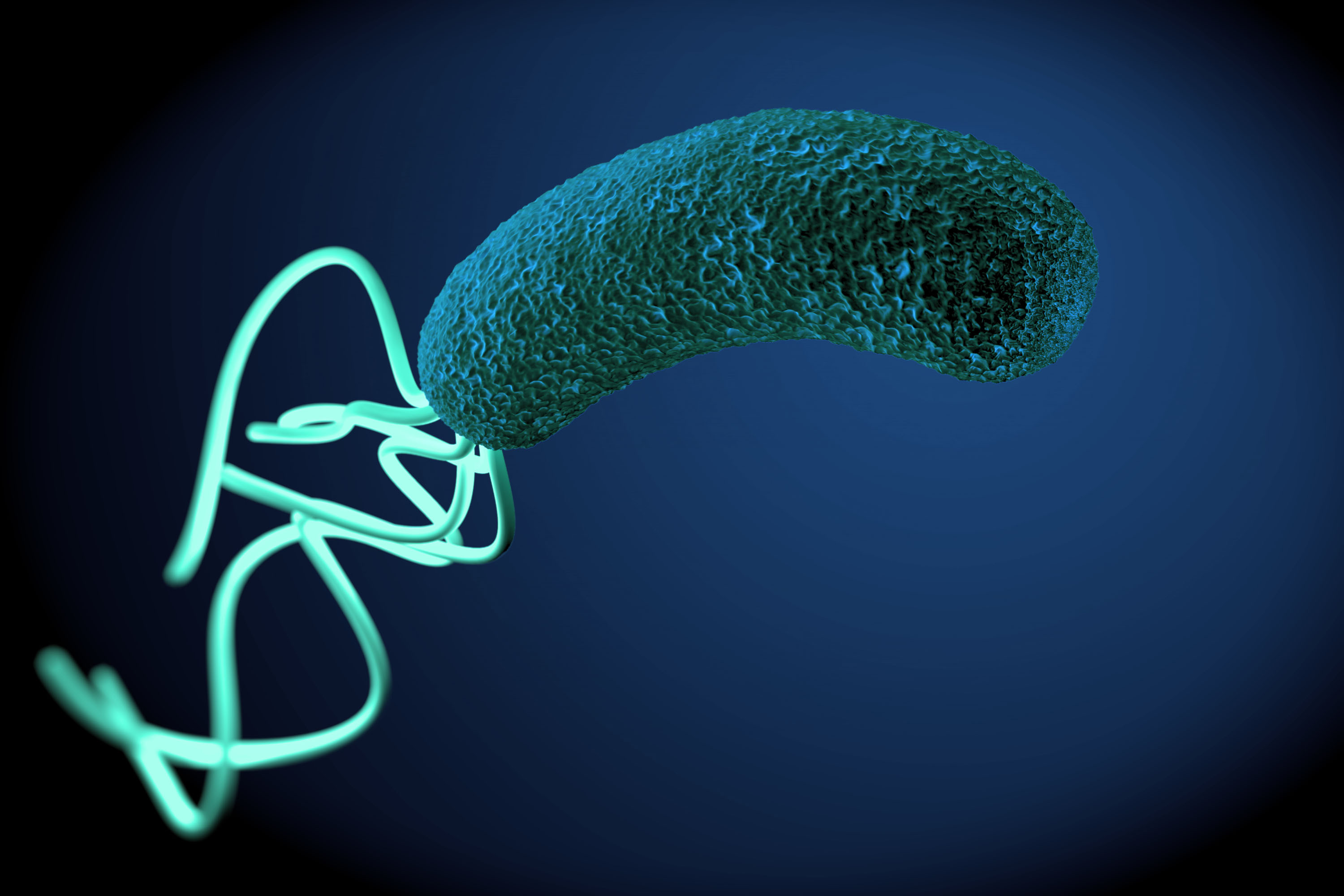
Infection with the ulcer bacterium Helicobacter pylori (H. pylori) has repeatedly been linked to Parkinson’s disease. Recently, researchers revealed that the infection is associated with higher levels of certain autoantibodies — possibly explaining the connection between the two seemingly unrelated disease states.
The research team at the University of Malaya, in Malaysia, have had a long-standing interest in the link between Parkinson’s and the gut bacterium. In 2014, they published the largest study to date that pointed to a link between the two conditions.
The new work, “Augmentation of Autoantibodies by Helicobacter pylori in Parkinson’s Disease Patients May Be Linked to Greater Severity,” recently published in the journal PLOS ONE, now reveals mechanisms that might explain the association.
The research team used an assay that measures antibodies to 1,636 human proteins in 30 Parkinson’s patients with confirmed H. pylori infections, and 30 infection-free patients of the same age and sex.
The assay revealed 13 autoantibodies that differed between the groups, eight of which were present at higher, and five at lower levels in the infected patients. Among the elevated autoantibodies, the study identified several antibodies targeting proteins with known functions in the brain.
One such protein, called NFIA, is a neuroprotective transcription factor. Lack of NFIA has been linked to a greater risk of nerve cell injury. Other proteins with brain connections were PDGFB, a growth factor linked to the regeneration of dopaminergic neurons, and the eIF4A3 protein, which is believed to play a role in learning and memory processes.
The majority of the identified antibodies target proteins without any known links to either gastric ulcers or Parkinson’s disease.
The authors of the study admit that it faced several limitations.
Researchers could not distinguish between an ongoing infection and previous exposure because the study used the presence of antibodies to H. pylori to identify the infection. Additionally, they did not know the ages of patients at infection, how long they carried the bacteria, and if patients had received treatment or not.
Such differences could explain why not all of the infected patients carried the antibodies. Future studies where autoantibody levels might be linked to severity of infection or virulence factors, are needed to better understand the connection between the seemingly unrelated conditions.


