1st transplant done in trial of Parkinson’s cell therapy ANPD001
Written by |
A Phase 1/2 clinical trial dubbed ASPIRO that’s testing Aspen Neuroscience’s ANPD001 — a stem cell therapy candidate designed to replace the nerve cells that are lost in Parkinson’s disease — has dosed its first patient.
A first transplant was conducted at the Banner-University Medical Center Tucson by neurosurgeon Paul Larson, MD, the trial’s lead investigator, Aspen announced in a company press release
ASPIRO (NCT06344026), which was cleared by the U.S. Food and Drug Administration (FDA) last year, is testing the long-term safety and tolerability of the ANPD001 stem cell therapy when transplanted at two escalating doses in people with moderate to severe Parkinson’s. The eligible study participants range in age from 50 to 70.
“The initiation of this clinical trial is a major milestone in Aspen’s mission to develop and deliver personalized, regenerative neurologic therapies for people with unmet medical needs, starting with Parkinson’s disease,” said Damien McDevitt, PhD, president and CEO of Aspen Neuroscience.
“To date, there is no disease-modifying therapy that can stop, replace or prevent the loss of dopamine neurons or slow the progression of Parkinson’s,” McDevitt said.
Additional trial goals will include assessments of the therapy’s early efficacy — by measuring so-called on time, or periods when a patient’s symptoms are controlled by medications — and the easing of motor symptoms. The trial is running at five clinical sites in the U.S.
ANPD001 designed to replace nerve cells lost in Parkinson’s
Parkinson’s is caused by the death of dopamine-producing neurons in the brain’s nigrostriatal dopaminergic pathway. That pathway includes the substantia nigra and the dorsal striatum, both involved in motor control. Dopamine is a major brain chemical messenger.
ANPD001 aims to replace the dopaminergic neurons that are lost in Parkinson’s.
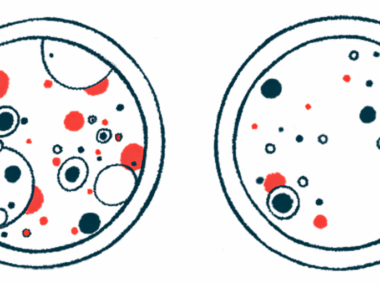
This experimental therapy for Parkinson’s uses a type of stem cell called an induced pluripotent stem cell, or iPSC, which is able to generate nearly any type of cell in the body — including dopamine-producing neurons. Its manufacturing is a three-step process.
The first step involves collecting skin cells from a patient, which are then modified in the lab and reprogrammed into iPSCs. The iPSCs are then provided with biochemical cues that guide them into transforming into dopamine neuronal precursor cells. These cells will eventually mature into dopamine-producing neurons once transplanted into patients.
The procedure is known as autologous because it uses a patient’s own cells.
“This is the first use of the autologous approach in a formal clinical trial,” said Larson, also a professor of neurosurgery at the University of Arizona College of Medicine-Tucson.
Larson called it “an honor” to take part in ASPIRO, saying it’s an “important study.”
“Parkinson’s disease is the most common neurodegenerative movement disorder, primarily affecting the depletion of dopamine neurons in the midbrain,” Larson said.
“By the time of diagnosis, it is common for people with Parkinson’s to have lost the majority of dopaminergic (DA) neurons in the nigrostriatal pathway, which leads to progressive loss of motor and neurological function,” Larson said.
Trial is first-in-human study of this Parkinson’s cell therapy
The enrolled participants — expected to be nine in total — were first remotely monitored via a digital health platform, by Rune Labs, as part of a Trial-Ready Cohort Screening study. The goal was to have a comprehensive view of the disease ahead of patient recruitment.
Also included in the trial’s additional goals, along with increased on time and reduced motor symptoms, is improvement in patients’ quality of life.
This first-in-human trial holds significant promise to investigate the ability of ANPD001 to improve the lives of people with moderate to advanced Parkinson’s disease.
The trial’s primary phase is expected to be completed by next year, and patients will be assessed for five years post-transplant, with the use of imaging scans of the brain.
“This first-in-human trial holds significant promise to investigate the ability of ANPD001 to improve the lives of people with moderate to advanced Parkinson’s disease,” said Edward Wirth III, MD, PhD, Aspen’s chief medical officer.
“Our 2022 Trial Ready Cohort Screening Study has completed enrollment, and we plan to dose patients in the ASPIRO Phase 1/2a study this year,” Wirth said.