Study in Small, Hospitalized Patient Group Sees No Added COVID-19 Risks
Written by |
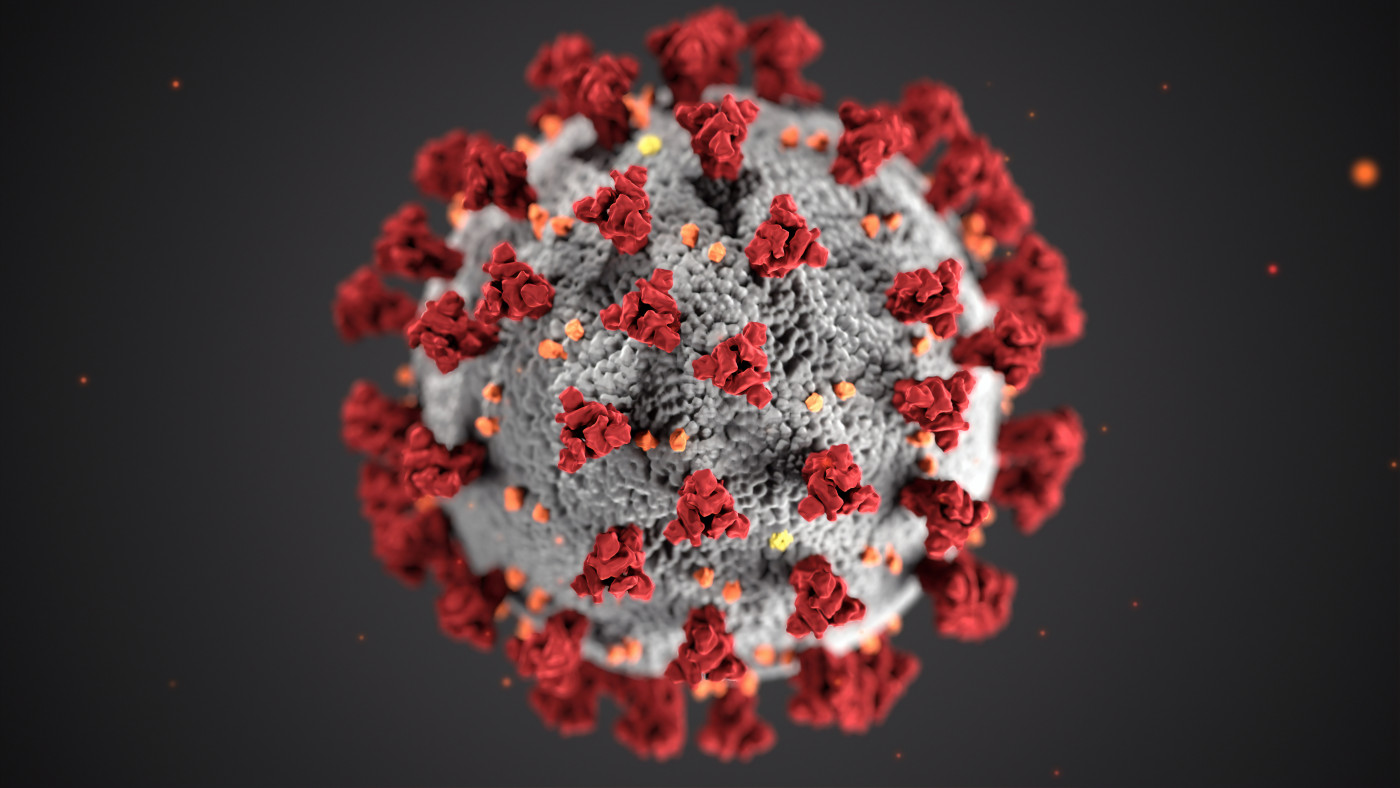
COVID-19-causing virus
Parkinson’s disease does not appear to make a person more susceptible to infection with the COVID-19-causing virus, or at risk of poorer outcomes, according to a study in a small hospitalized patient group in Italy when the pandemic struck.
The observational study, “The impact of SARS-COV2 infection on people in residential care with Parkinson Disease or parkinsonisms: Clinical case series study,” was published in PLOS One by a team of researchers from Italy.
COVID-19 is an infection caused by the SARS-CoV-2, or severe acute respiratory syndrome coronavirus 2, virus. Previous studies suggested that people with chronic diseases like Parkinson’s, and the advancing age that is common to this disorder, may be more vulnerable to infection by SARS-CoV-2.
Researchers looked at data covering 18 people admitted to the rehabilitation unit of a hospital in Messina about an average of 30 days before the COVID-19 outbreak was declared a pandemic on March 11, 2020, by the World Health Organization.
Their aim was “to evaluate the susceptibility of patients with Parkinson’s disease and parkinsonisms to develop the disease, and how the infection may influence the risk of clinical worsening and increase of mortality,” the team wrote.
Among these 18 patients (eight men and five women), 13 had Parkinson’s disease and the remaining five had other neurological diseases. This group’s overall mean age was 65; the average age among those with Parkinson’s was 68, and their average disease duration was 9.15 years.
After SARS-CoV-2 infection was reported in the unit, throat swabs were given to check patients’ status. The test came back positive in 10 (77%) Parkinson’s patients (six men and four women), and in three (60%) men with non-Parkinson’s neurological diseases.
Everyone in this study was followed for up to seven days after COVID’S onset in the rehab unit, at which time they were transferred elsewhere.
Five of the infected Parkinson’s patients (three women and two men) were asymptomatic, and another four (40%, one woman and three men) had mild symptoms, such as fever, muscle pain, and inflammation of the pharynx, the study reported.
Symptoms like fever and respiratory difficulties were serious in the one other Parkinson’s patient, a 67-year-old man diagnosed 12 years earlier, and he required oxygen treatment. All three infected men with other neurologic disorders — one each with stroke, mild cognitive impairment, and spinal degeneration — were symptomatic, and two also needed oxygen due to pneumonia.
People in the Parkinson’s group were receiving treatment with levodopa, with daily doses ranging from 100 to 950 mg. Those who tested positive for SARS-CoV-2 did not differ from in age, disease duration, or levodopa daily dose from those who tested negative.
“Our findings seem to report that PD [Parkinson’s disease] shouldn’t be considered as a risk factor for SARS-COV2 infection, even if our sample demonstrated clearly the vulnerability of Rehabilitative Unit that allowed the spread of the infection,” the researchers wrote.
With infected patients, use of Parkinson’s medications like levodopa should be continued to help ease bradykinesia (slowed movements) and rigidity that could affect respiration, they added.
Longer studies in larger groups are needed “to evaluate the actual susceptibility of patients with Parkinson’s disease to develop COVID-19 disease, and how the infection may influence the risk of clinical worsening and … mortality,” the researchers concluded.




