Antibody-based Therapies May Trigger Brain Inflammation
New research suggests that brain inflammation is the likely reason antibody-based therapies are ineffective in clinical trials for people with Parkinson’s and Alzheimer’s diseases.
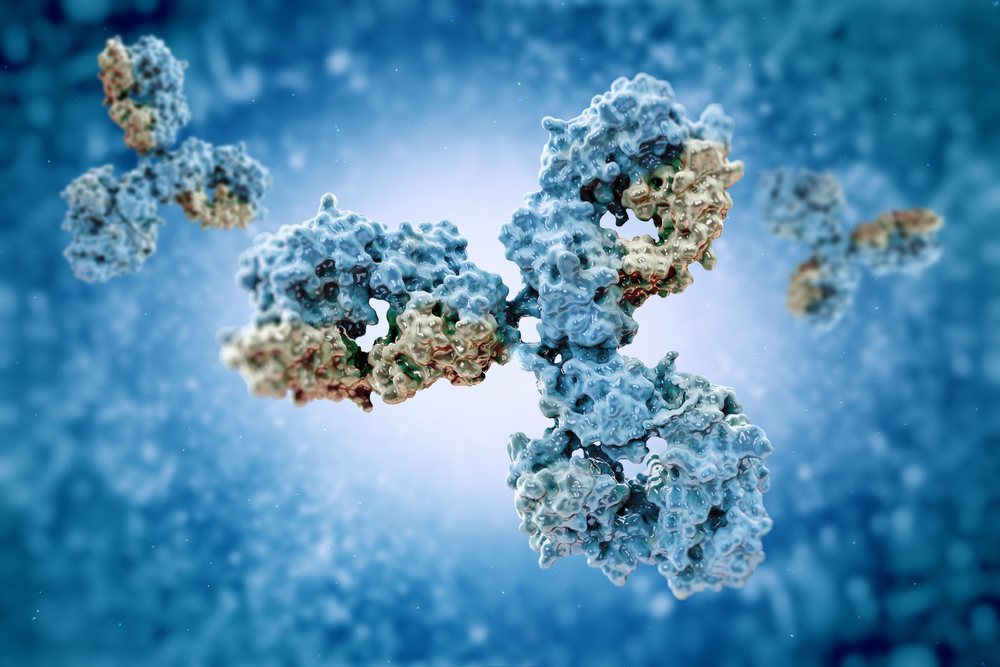
The findings show that the binding of the antibody to its target protein — in the case of Parkinson’s disease the misfolded alpha-synuclein — trigger a pro-inflammatory state in human microglial cells, which are the immune cells of the central nervous system (CNS).
“Our findings provide a possible explanation for why antibody treatments have not yet succeeded against neurodegenerative diseases,” Stuart Lipton, MD, PhD, co-director of the Neurodegeneration New Medicines Center at The Scripps Research in La Jolla, California, and the study’s lead author, said in a press release.
The study “Soluble α-synuclein/antibody complexes activate the NLRP3 inflammasome in hiPSC-derived microglia” will be available soon in the journal Proceedings of the National Academy of Sciences.
Both Parkinson’s and Alzheimer’s disease are characterized by the formation of protein clumps, also called aggregates, which are thought to drive disease progression. In Parkinson’s, these aggregates are composed mostly of misfolded (abnormally shaped) alpha-synuclein; in Alzheimer’s, they are made up of mostly amyloid-beta protein.
In both cases, small aggregates of these proteins, called oligomers, are considered particularly harmful to nerve cells.
By developing antibodies targeting these protein clumps, researchers reasoned it would stop the spread of protein aggregates in the brain, which would slow disease progression.
While the mechanism as to why these aggregates fuel disease progression remains elusive, research suggests that inflammation may play a role.
Researchers now have found that alpha-synuclein clusters (oligomers) induce an inflammatory state in human microglia cells, but that therapeutic antibodies against alpha-synuclein worsen this inflammation. Microglia cells are responsible for maintaining an immune cell balance in the brain, and are capable of releasing pro- and anti-inflammatory signals in response to changes in the brain’s microenvironment.
They discovered the brain inflammation was not being caused by the antibodies themselves, but rather by the complexes made of antibody and target protein.
Since in Parkinson’s and Alzheimer’s disease two protein aggregates often coexist — both alpha-synuclein and amyloid-beta — researchers added amyloid beta oligomers to microglia cells that were already exposed to alpha-synuclein, to reflect what would happen normally in patients’ brains.
The results showed that this worsened inflammation, however, and adding antibodies targeting the anti-amyloid beta worsened it even more. In fact, the team found that the successful targeting of the antibody toward its protein always made inflammation worse.
The researchers used human-derived microglial cells, either in lab tests or injected into mice whose immune systems were manipulated beforehand not to attack the cells. However, previous studies testing the experimental antibodies used mouse microglial cells.
Researchers believe this is a better model to study therapeutic antibodies because, unlike human clinical trials, studies in mice have shown a positive response to these antibodies.
“We see this inflammation in human microglia, but not in mouse microglia, and thus this massive inflammatory effect may have been overlooked in the past,” said Lipton.
The researchers believe the activation of the human microglial cells is the lijely reason these type of antibodies have been ineffective in clinical trials.
Lipton and his colleagues have devolved an experimental treatment that may help lessen this antibody-induced brain inflammation, restoring its therapeutic effect. More studies are planned.






