Parkinson’s Patients Have Many More Opportunistic Microbes in Their GI Tract, Study Reveals
Written by |
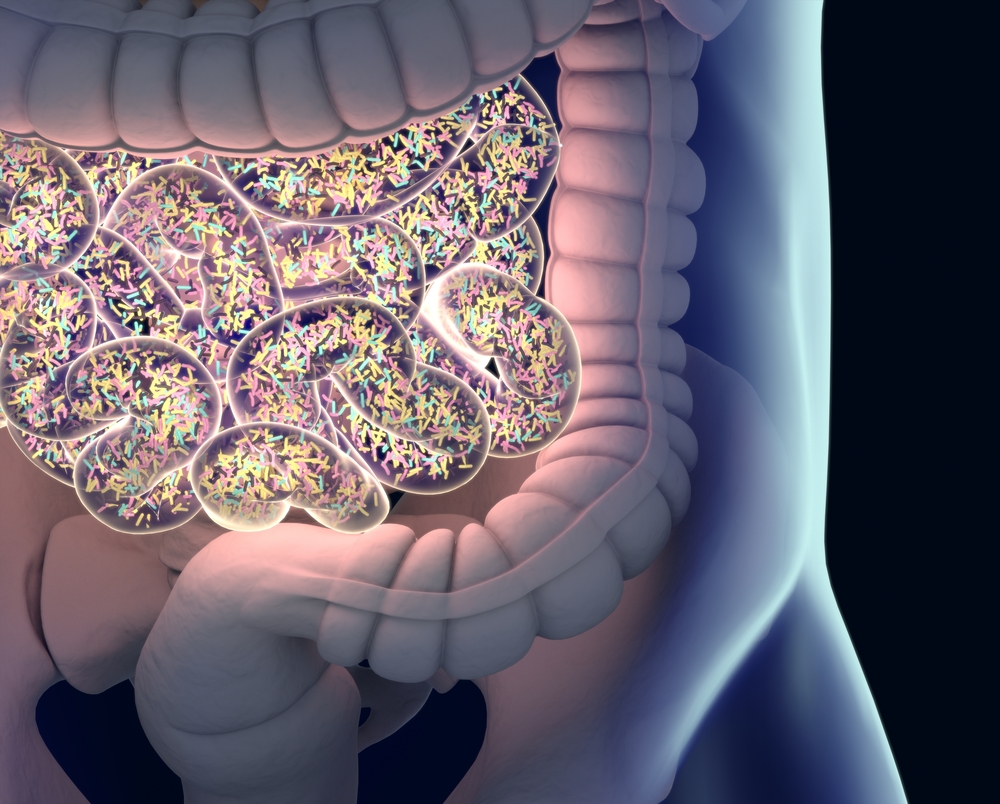
Scientists have discovered, for the first time, that patients with Parkinson’s disease have a much greater number of opportunistic disease-causing microbes living in their gastrointestinal tract, compared to people without the disease.
Further studies are needed to determine if these opportunistic microorganisms may be involved directly in the onset and development of the disease, researchers noted.
The study, “Characterizing dysbiosis of gut microbiome in PD: evidence for overabundance of opportunistic pathogens,” was published in the Nature Partner Journal Parkinson’s Disease.
Although the specific causes of Parkinson’s are still not fully understood, it is believed the disease results from a combination of genetic and environmental factors.
In 2003, German researchers led by Professor Heiko Braak proposed that non-inherited forms of Parkinson’s actually develop first in the gut, driven by the presence of harmful microbes that then travel to the brain using the network of nerves that innervate the gastrointestinal (GI) tract, called the enteric nervous system.
“Although many aspects of Braak’s hypothesis have gained support in recent years, there is no direct evidence that a pathogen [disease-causing microbe] is involved,” researchers wrote.
However, researchers from the University of Alabama at Birmingham and colleagues now have found that individuals with Parkinson’s have a much higher number of opportunistic pathogens living in their GI tract, compared to people without the disease.
“The exciting question is whether these are Braak’s pathogens capable of triggering PD [Parkinson’s disease], or are they irrelevant to PD but able to penetrate the gut and grow, because the gut lining is compromised in PD,” Haydeh Payami, PhD, professor of neurology at the University of Alabama at Birmingham, said in a news story.
Normally, opportunistic microbes are harmless. However, under certain circumstances they may become dangerous and cause infections, particularly in those who have a compromised immune system, or a disorder that disrupts their gut lining.
Although previous studies reported a series of alterations in the composition of microorganisms found in the GI tract of patients with Parkinson’s, these opportunistic microbes have never been found before.
“We suspect the reason we were able to detect these microorganisms is that they are rare and we had a much larger sample size and power than prior studies,” Payami said.
Payami and her colleagues carried out the largest microbiome-wide association study — studies that aim to determine if certain microbes can be associated with a specific disorder — in patients with Parkinson’s to date.
Using advanced gene sequencing and bioinformatic tools, they analyzed data from two independent datasets: one containing data from 197 individuals with Parkinson’s and 130 individuals without the disease (controls); and another containing data from 323 Parkinson’s patients and 184 controls.
Consistent with previous studies, their analyses revealed that compared to controls, patients with Parkinson’s had much higher numbers of carbohydrate-metabolizing probiotic bacteria belonging to the Lactobacillus and Bifidobacteria genera in their GI tract.
Conversely, and also in agreement with previous studies, patients had lower numbers of microbes that produce short-chain fatty acids, including several belonging to the Ruminococcaceae and Lachnospiraceae families.
Analyses also showed, for the first time, that patients with Parkinson’s had much higher levels of opportunistic microbes in their GI tract compared to controls, including those belonging to the Porphyromonas, Prevotella, and Corynebacterium genera.
Importantly, the 15 bacteria genera that were found to be associated with Parkinson’s disease were observed in both datasets. Alterations in gut bacteria composition seen in patients with Parkinson’s was found to be independent of sex, age, body mass index (BMI), level of GI discomfort, diet, and geographical region.
“In conclusion, we uncovered robust and reproducible signals, which reaffirm and generate leads for experimentation into cause and effect, disease progression, and therapeutic targets,” the researchers wrote.
“There is more to be learned with larger sample sizes with greater power, longitudinal studies to track change from prodromal [early] to advanced disease, and by next-generation metagenome sequencing to broaden the scope from bacteria and archaea to include viruses and fungi, and improve the resolution to strain and gene level,” they added.





