Changes in Neuronal Communication Linked to Falls and Freezing of Gait in Parkinson’s, Study Finds
Parkinson’s disease-related falls and freezing of gait — when patients are unable to move their feet forward when trying to walk — are associated with changes in a specific type of neuronal communication in different brain regions, a study reports.
The study, “Cholinergic system changes of falls and freezing of gait in Parkinson disease,” was published in Annals of Neurology.
Many people with Parkinson’s disease will experience falling and freezing of gait, which tend to become more frequent as the disease progresses. In some cases, symptoms cannot be controlled with dopaminergic therapy, suggesting that non-dopamine mechanisms contribute to Parkinson’s disease motor symptoms.
Previous studies have shown that the brainstem and basal forebrain regions with degenerated acetylcholine-releasing neurons traveling to the thalamus and cerebral cortex are associated with falls and slow gait speed in Parkinson’s patients.
The brainstem is the region of the brain that is continuous to the spinal cord, and the basal forebrain is important in the production of acetylcholine, which is a neurotransmitter released by nerve cells to send signals to other cells (neurons, muscles, and glands). The thalamus is involved in several important processes, including consciousness, sleep, and sensory interpretation; the cerebral cortex plays a key role in memory, attention, perception, awareness, thought, language, and consciousness.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Join today!
Scientists have also observed reduced dopaminergic nerve terminals in the striatum, reduced cholinergic (meaning “acetylcholine-releasing”) nerve terminals in the cortex, and more severe beta-amyloid accumulation in Parkinson’s disease “freezers” compared with “non-freezers.”
The striatum coordinates multiple aspects of cognition, including both motor and action planning; the cholinergic system contains nerve cells that use acetylcholine to propagate a nerve impulse, and has been associated with a number of cognitive functions, including memory, selective attention, and emotional processing.
University of Michigan researchers hypothesized that distinct patterns of cholinergic projection system changes in the brain are associated with freezing of gait and falls in Parkinson’s patients.
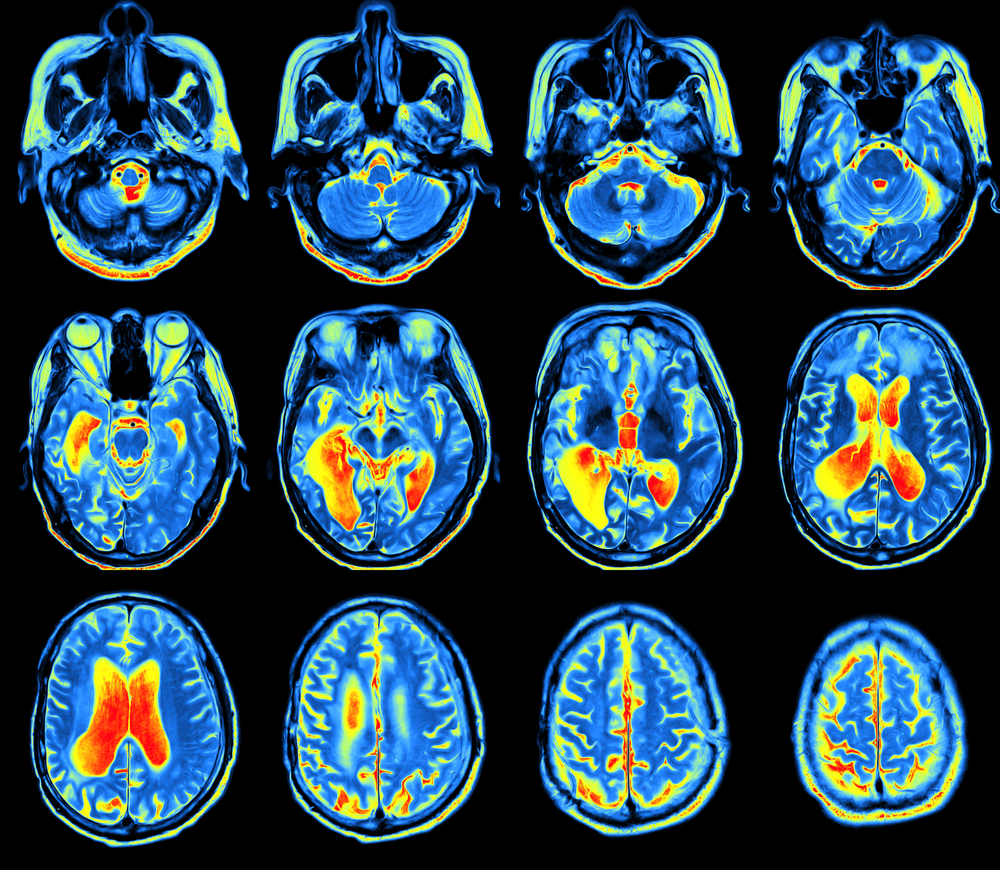
The team examined and performed [18F]FEOBV positron emission tomography (PET) scans on 94 Parkinson’s patients (72 men and 22 women) with a history of falling and “freezing.” Most subjects were taking dopamine agonists, carbidopa-levodopa or combinations of both.
[18F]FEOBV is a radioactive marker that selectively binds to the vesicular acetylcholine transporter (VACht) that loads acetylcholine into synaptic vesicles — sac-like structures in neurons that store chemical messengers before releasing them into the gap between nerve cells (synapse), enabling neuronal communication.
A PET scan is a non-invasive imaging technique to visualize metabolic processes in the body. Before the scan, [18F]FEOBV is administered via injection; doctors wait for the radiotracer to be distributed throughout the body, and then scan the patient to detect and quantify the patterns of its accumulation in the body.
Because the marker binds to VACht, scientists use it to quantify active cholinergic nerve terminals in the brain.
“Participants were asked about a history of falling. A fall was defined as an unexpected event during which a person falls to the ground. The presence or absence of (freezing of gait) was based on clinical examination and directly observed by the clinician examiner,” according to The Movement-Disorder Society Sponsored-Unified Parkinson’s Disease Rating Scale (MDS–UPDRS), the researchers wrote.
They reported that 35 participants (37.2%) had a history of falls, and 15 (16%) had observed freezing of gait.
Compared with non-fallers, fallers had a significant decrease in VACht expression within the right thalamus, specifically in the lateral geniculate nucleus, which is the primary center for processing visual information. This suggests that the visual information processing required for walking around safely might be compromised in Parkinson’s patients with a history of falling.
On the other hand, patients with freezing of gait had significantly reduced VACht expression in the bilateral striatum and hippocampus — required for learning and memory — compared with non-freezers.
The team found that a history of falls was associated with cholinergic projection system changes that relay to the thalamus, while the neural signals behind freezing of gait transmit to the caudate nucleus — a brain region associated with motor processing.
They also found that Parkinson’s fallers had a lower density of thalamic cholinergic nerve terminals compared with non-fallers.
Freezing of gait was related to longer disease duration, more severe parkinsonian motor ratings, and higher levodopa levels.
These results suggest that changes in acetylcholine-mediated neuronal communication are linked to falls or freezing behavior, depending on the affected brain region.






