Inflammatory Bowel Disease Linked to Risk of Parkinson’s in Large Review Study
People with inflammatory bowel disease (IBD), an umbrella name for disorders marked by prolonged inflammation of the digestive tract, are at a higher-than-usual risk for Parkinson’s disease, a review study involving 8.9 million IBD patients suggests.
The study, “The risk of Parkinson’s disease in inflammatory bowel disease: A systematic review and meta-analysis,” was published in the journal Digestive and Liver Disease.
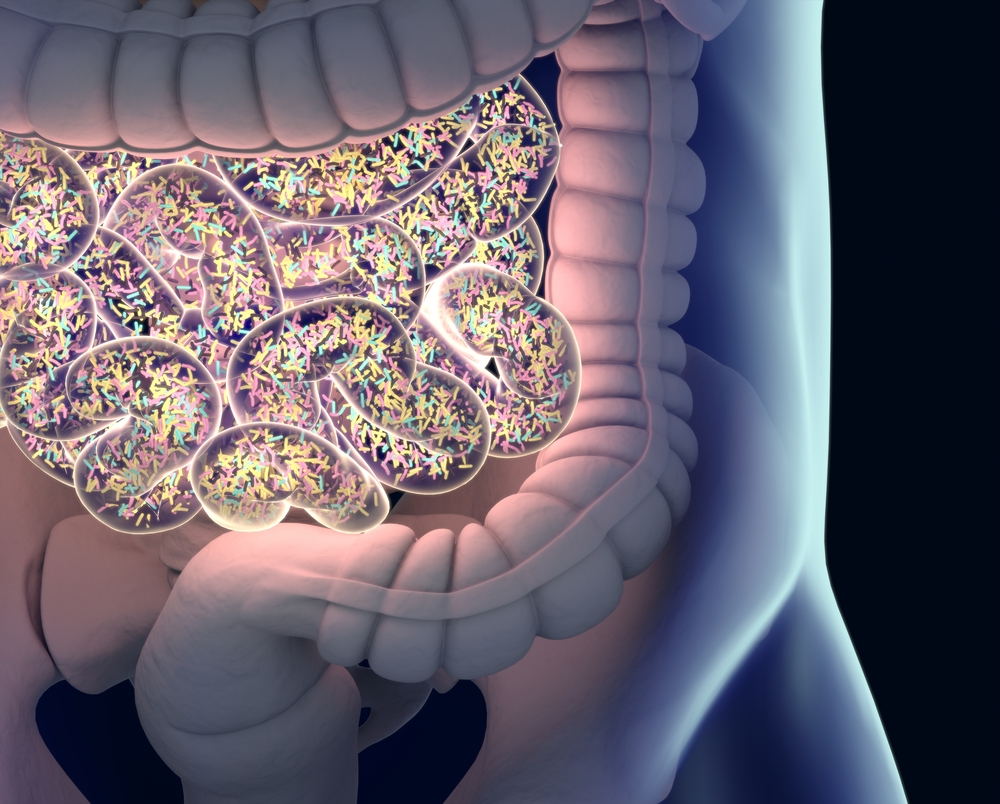
Inflammatory bowel disease (IBD) is a term that includes two main disorders — ulcerative colitis and Crohn’s disease — and is characterized by an imbalanced immune response that triggers prolonged inflammation of the digestive tract.
Inflammation in ulcerative colitis is confined to the colon (large intestine), while in Crohn’s disease it can involve any part of the digestive system. But inflammation in Crohn’s is most common at the end of the ileum (the last section of the small intestine) or the colon.
Several studies have reported that some of the inflammatory pathways impaired in Parkinson’s are also found in IBD. Certain population-based studies have also reported an increased prevalence of Parkinson’s among IBD patients, but the link between both disorders remains controversial. Another follow-up study failed to confirm those initial findings.
Want to learn more about the latest research in Parkinson’s Disease? Ask your questions in our research forum.
Researchers in China conducted a meta-analysis of published literature focusing on Parkinson’s risk in IBD using two databases, PubMed and Embase, and including in their search the keywords “ulcerative colitis” and “Crohn’s disease.” For the meta-analysis, they included cohort or case-control studies with patients diagnosed with IBD, either ulcerative colitis and Crohn’s disease, and whose main outcome was Parkinson’s.
Out of an initial pool of 172 studies, four studies accounting for a total of more than 8.9 million patients were included in the meta-analysis. (A meta-analysis is a statistical technique used to summarize in a quantitative manner the findings of multiple studies.)
Performed in the United States, Denmark, Sweden and Taiwan, these four studies assessed the incidence rate of Parkinson’s in IBD patients, specifically those with Crohn’s and ulcerative colitis. Three had been conducted in 2018, and one in 2016.
“To our knowledge, this is the first MA [meta-analysis] to focus on the risk of PD [Parkinson’s] in IBD patients,” the research team wrote. “Despite the small number of studies included, the patient numbers were large due to the population-based nature of the included studies.”
Pooled results of all studies suggested that an IBD diagnosis was associated with a 41% increased risk of developing Parkinson’s.
Assessing the risk of ulcerative colitis and Crohn’s disease separately, researchers found that both disease subtypes were linked to a higher Parkinson’s risk compared with age- and sex-matched controls — Crohn’s patients had a 28% higher risk of Parkinson’s, and those with ulcerative colitis a 30% increased risk, the study reported.
Among the IBD patients, the risk for Parkinson’s was not affected by gender, with similar rates seen in male and female patients, or by age.
Overall, this meta-analysis “identified an increased risk of PD in IBD patients,” the reseachers wrote, which “remained significant when separately analysing CD [Crohn’s disease] and UC [ulcerative colitis] subgroups.”
“More comprehensive and detailed MA using a larger number of studies are required to validate our findings in the future,” the study concluded.