Tiny Brain Bleeds Associated with Parkinson’s Disease Dementia, Study Reports
Written by |
Tiny bleeds in the brain are associated with cognitive impairment in Parkinson’s disease and risk of Parkinson’s disease dementia (PDD), a Japanese study has found.
The research, “The presence of cerebral microbleeds is associated with cognitive impairment in Parkinson’s disease,” was published in the Journal of Neurological Sciences.
Cerebral microbleeds (CBMs) are small, chronic brain hemorrhages likely caused by structural abnormalities of the small vessels in the brain. CBMs are markers of small vessel disease frequently found in normal aging, as well as in patients with stroke and Alzheimer’s disease. These lesions are known promoters of cognitive decline in the elderly and are linked to poor prognosis in Alzheimer’s patients.
Cognitive impairment is one of Parkinson’s non-motor symptoms and, along with dementia, affects Parkinson’s prognosis. Other non-motor symptoms – including visual hallucinations, sleep problems, behavior disorders, and orthostatic hypotension (a decrease in blood pressure when standing up), as well as older age at onset — are considered risk factors for Parkinson’s cognitive decline.
The authors previously had shown that CBMs are common in Parkinson’s patients. Also, experimental studies reported that brief brain blood flow reduction promotes the aggregation of alpha-synuclein protein, a key player in Parkinson’s disease.
However, whether the presence of these lesions is a risk factor for cognitive impairment in patients with Parkinson’s was not clear.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
Juntendo University researchers retrospectively analyzed a total of 124 clinically diagnosed Parkinson’s patients to determine the association between the presence of CBMs and cognitive decline. Both early-stage and advanced disease cases were included.
Twenty-one patients (16.9%) were diagnosed with PDD. Factors including gender, age, Hoehn and Yahr (H-Y) stage (a system used to assess the worsening of Parkinson’s symptoms) history of stroke, orthostatic hypotension (defined as a 20-mm Hg drop in systolic and/or a 10 mm Hg drop in diastolic blood pressure), systolic hypertension (systolic blood pressure equal to or higher than 140 mm Hg), specific cerebrovascular lesions, and the use of oral blood thinners. All significantly correlated with PDD.
Matching prior findings, abnormal nocturnal blood pressure — increasing or falling 10 to 20% — also was associated with PDD.
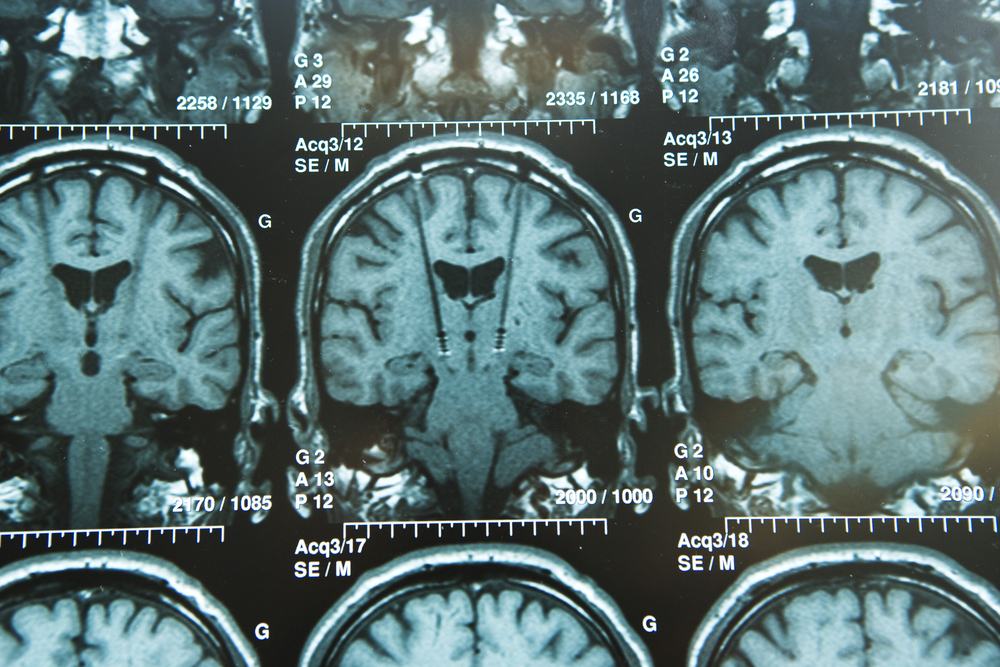
CBMs — defined by brain MRI as having a diameter of 2-10 mm — were observed more frequently in PDD patients than in those without dementia. This finding was maintained across different microbleeds’ types called deep or infratentorial (below the brain lobes) and strictly lobar (restricted to the brain lobes).
Interested in Parkinson’s Disease research? Sign up for our forums and join the conversation!
Also, both types of CBMs were associated with lower cognitive scores, as measured with the Mini-Mental State Examination (MMSE) and the Hasegawa dementia scale-revised. Patients with a strictly lobar type of microbleed scored lower on both scales than individuals with deep or infratentorial ones.
Patients with CBMs were older and had a higher (worse) H-Y stage than those without these lesions. They also showed more severe cerebrovascular lesions and higher prevalence of hypertension, diabetes mellitus, history of ischemic stroke, coronary artery disease, orthostatic hypotension, systolic hypertension, and use of oral blood thinners and anti-hypertensive medications.
Importantly, male gender, cerebrovascular lesions on MRI, and strictly lobar CMBs (but not deep and infratentorial) were risk factors for PDD.
“In conclusion, CMBs, especially strictly lobar type, are associated with cognitive decline and dementia in [Parkinson’s],” researchers wrote.
Amyloid plaques — typical in Alzheimer’s patients’ brains — are known contributors for cognitive decline in Parkinson’s and are more common in PDD patients than in those with Parkinson’s but not dementia. In fact, up to 50% of patients with PDD also may have an Alzheimer’s pathology.
“[O]ur data suggest that [Parkinson’s] cases with strictly lobar distribution of CMBs may have an underlying [Alzheimer’s] pathology and contribute to cognitive decline,” the scientists added.
However, the research team noted that future studies with larger patient groups are necessary to confirm these results.




