Deep Brain Stimulation Surgery Works Better If Patients Are Asleep, Study Suggests
Deep brain stimulation surgery, used to treat the effects of Parkinson’s disease, is performed better when patients are asleep rather than awake, researchers from the Oregon Health & Science University (OHSU) suggested in a recent study comparing the two surgical settings.
The study could influence how the procedure is performed around the world, as patients are given the opportunity to reduce their symptoms without the need for experiencing a six-hour brain surgery while awake.
“It doesn’t take a rocket scientist, or a brain surgeon, to tell you that patients prefer it,” Kim Burchiel, MD, professor of neurosurgery at the OHSU School of Medicine and senior study author, said in a press release.
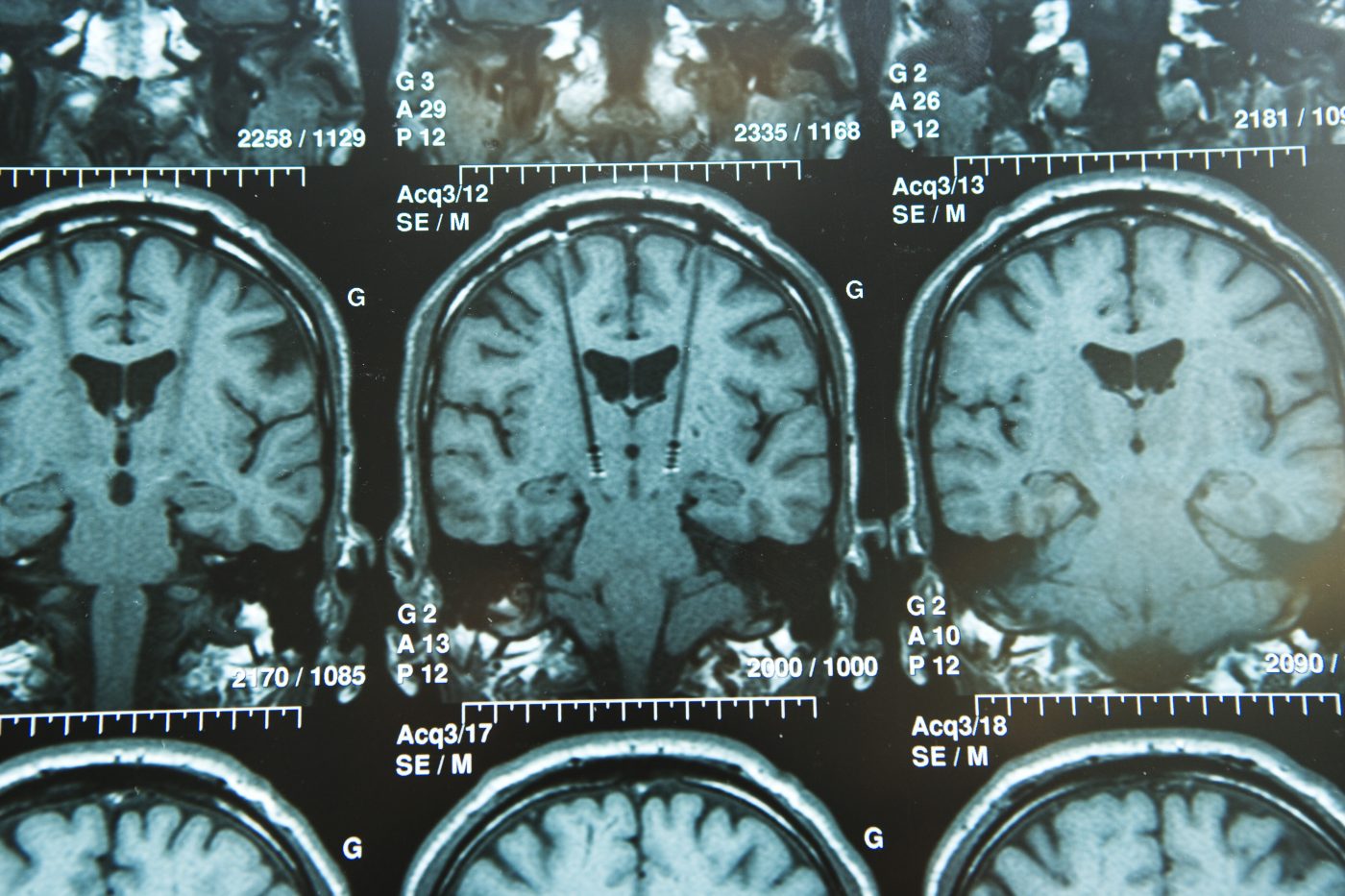
The practice of keeping patients awake during this type of surgery stems from the need to accurately place electrodes in the brain of a Parkinson’s patient. These electrodes stimulate nerve cells to reduce movement symptoms of the disease, but they need to be precisely located to do their work.
Until now, the gold standard for deep brain stimulation surgery has been the use of so-called microelectrodes. These map out the boundaries of the targeted brain structure. Initial measurements are also used to assess if the stimulation is effective or if it causes side effects before the surgery is completed.
Better brain imaging methods have made it possible to identify the correct brain structure without the need for placing these microelectrodes. This, in turn, allows patients to be asleep during the procedure.
In the study, “Clinical outcomes of asleep vs awake deep brain stimulation for Parkinson disease,” OHSU researchers compared the outcomes of patients who had the procedure while asleep with those who had traditional surgery while awake in a clinical trial (NCT01703598).
In 2011, OHSU switched to the new procedure and compared outcomes among patients operated on in 2010 with those who had electrodes implanted later. Burchiel performed all 69 surgeries in the study.
The results, published in the journal Neurology, suggested that it is better for patients to sleep through the surgery.
Additionally, traditional forms of deep brain stimulation surgery often cause patients to lose speech fluency. Matthew Brodsky, MD, an associate professor of neurology at the OHSU School of Medicine and medical director of OHSU’s deep brain stimulation program, believes that this side effect could be related to the use of microelectrodes.
Using microelectrodes, surgeons need to perforate the brain twice — once with the microelectrodes and again to position the electrode and battery pack that will remain in the brain.
“Patients undergoing asleep-DBS [deep brain stimulation] had improved speech versus patients undergoing awake DBS, whose speech fluency predictably worsened,” said Brodsky, who is the lead author of the study.
Meanwhile, improvements in Parkinson’s symptoms were similar in the two groups.
“If the patient’s outcome is not better or at least the same as awake-DBS, then you shouldn’t be doing it,” Burchiel said. “This article is really a watershed because we’re in a position to say, why would you ever do an awake surgery if you can get the same results or better when the patients are asleep – and the patients’ satisfaction is dramatically better?”
In an accompanying editorial, two scientists from the U.K. concluded that the study shows that the use of imaging in asleep patients will reduce risks without mitigating outcomes. They also underscored that the asleep procedure is faster and cheaper than the method used in awake patients.
Instead, the use of microelectrodes should be reserved for use in a research setting, they wrote.
While asleep deep brain stimulation surgery is not performed at many clinics outside of OHSU, Burchiel thinks his clinic will soon be joined by others as neurosurgeons realize the benefits of the newer procedure.






