Aberrant Astrocytes May Lead to Parkinson’s, Other Neurodegerative Diseases
Written by |
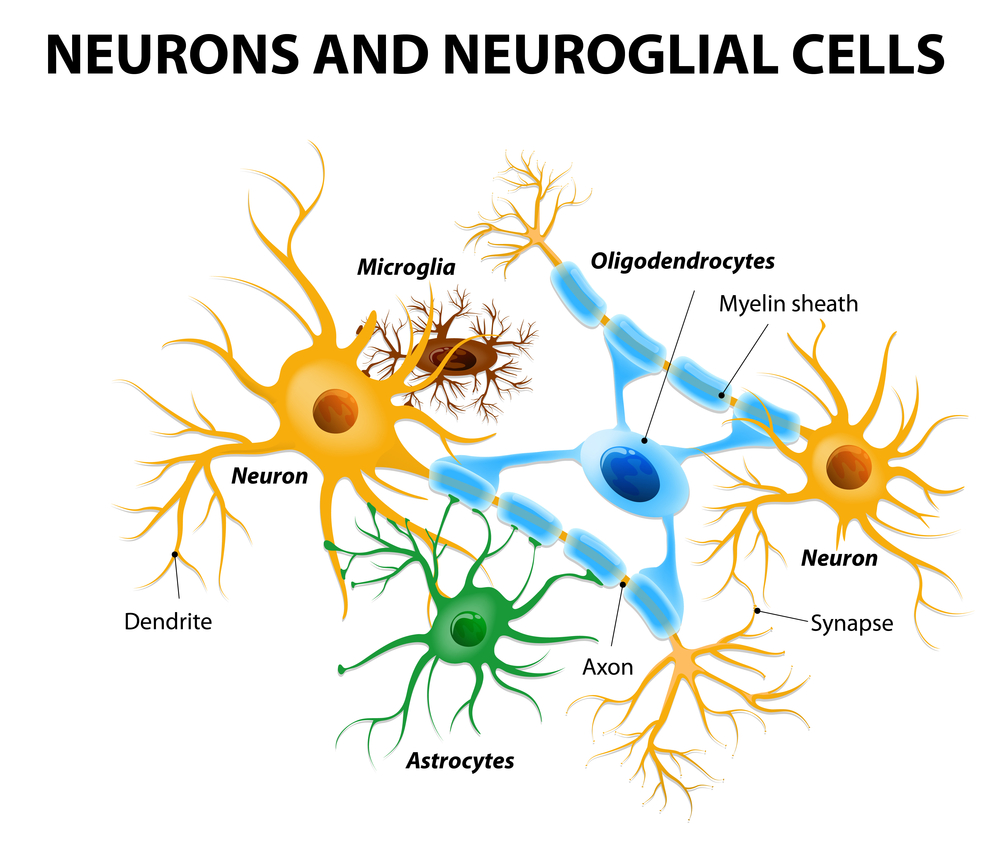
Astrocytes are brain cells usually known for their protective role toward neurons in various conditions, such as stroke and spinal cord injury. Researchers have now found they also can exert a damaging effect in neurons under certain circumstances and lead to several diseases, such as Parkinson’s.
The research work establishes that astrocytes turn bad in the presence of certain inflammatory molecules produced by microglia, immune cells with a crucial role in the defense of the central nervous system.
The study, “Neurotoxic Reactive Astrocytes Are Induced By Activated Microglia,” was published in the journal Nature.
“We’ve learned astrocytes aren’t always the good guys,” Ben Barres, MD, PhD and senior author of the study, said in a news release. “An aberrant version of them turns up in suspicious abundance in all the wrong places in brain-tissue samples from patients with brain injuries and major neurological disorders from Alzheimer’s and Parkinson’s to multiple sclerosis. The implications for treating these diseases are profound.”
He believes that therapeutic approaches that target the conversion of astrocytes into “the bad guys” or that block their damage in neurons may be efficient to stop the development of neurological diseases.
Previous studies by Barres and his team had shown that there are two types of reactive astrocytes, which they named A1 and A2. While A1 astrocytes produce large amounts of inflammatory molecules, A2, which are induced by strokes, for example, produce molecules that help the affected neurons survive.
Researchers found that the presence of LPS, a molecule produced by bacteria, induced the conversion of normal astrocytes into the A1 type, thereby promoting inflammation. They also found that microglia, the brain’s immune cells that are also activated by LPS, could induce astrocytes’ transformation into the A1 type by releasing inflammatory molecules.
In the new study, the team used mice to identify molecules produced by microglia that change astrocytes’ behavior in the presence of LPS: TNF-alpha, IL-1-alpha, and C1q. While each of these substances could partially induce A1 astrocytes, when combined, they promote the complete transformation of astrocytes. When fully formed, A1 astrocytes no longer feed and protect neurons, but instead kill them.
In another experiment, researchers used retina cells that only survive in culture when surrounded by astrocytes that feed and protect them. They saw that in the presence of normal astrocytes, these retina cells would growth and mature, but in the presence of A1 astrocytes, they would become weak and faulty. These neurons would even die when in the presence of increasing amounts of the killing molecules produced by A1 astrocytes.
Similar results were seen when other types of neurons, such as dopaminergic neurons (whose loss is involved in Parkinson’s disease), were put in contact with A1 astrocytes’ products.
Importantly, researchers found that mice in which the optic nerves had been damaged (a trigger that kills retina cells) had increased amounts of A1 astrocytes, but that inhibiting TNF-alpha, IL-1-alpha, and C1q with antibodies prevented A1 formation and protected these neurons.
Brain samples from patients with Alzheimer’s, Parkinson’s, and Huntington’s diseases, amyotrophic lateral sclerosis (ALS) and multiple sclerosis were also found to have high quantities of A1 astrocytes that accumulated in the regions most affected by the disease.
Researchers are currently trying to identify exactly which molecules produced by A1 astrocytes have the observed killing effect in neurons.
“We’re very excited by the discovery of neurotoxic reactive astrocytes,” Barres said, “because our findings imply that acute injuries of the retina, brain and spinal cord and neurodegenerative diseases may all be much more highly treatable than has been thought.”





