Parkinson’s Might Be Treatable via Stem Cell Therapy
[Parameter-Settings] FileVersion = 2000 Date/Time = 0000:00:00 00:00:00 Date/Time + ms = 0000:00:00,00:00:00:000 User Name = TCS User Width = 1140 Length = 956 Bits per Sample = 8 Used Bits per Sample = 8 Samples per Pixel = 3 ScanMode = xy Series Name = 04.16.12.lei
Interest in the potential of stem cell therapy to treat a variety of neurological conditions, including Parkinson’s disease (PD), has been growing for several years, but the question remains: how close are these treatments to clinical use? A new article in the journal Acta Neurologica Scandinavica explored whether stem cell therapy is a viable and realistic approach for replacing neurons lost to diseases like PD, and concluded that more research is needed.
The article, “Current status of treating neurodegenerative disease with induced pluripotent stem cells,” comes from researchers at Aarhus University in Denmark.
PD is caused by death of dopamine-producing cells in a brain region called the substantia nigra, hampering movement. Current treatments focus primarily on replacing the lost dopamine, but these treatments eventually fail because the dopamine-making cells continue to die. For this reason, stem cell therapy is of interest.
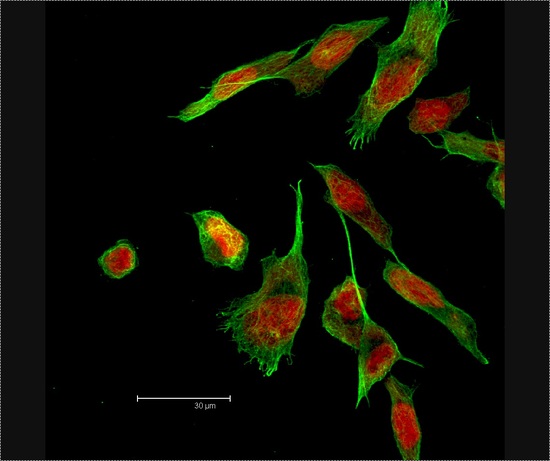
According to the researchers, “Over recent years, the potential of induced pluripotent stem cells (iPSCs) has been widely investigated and these cells seem promising for production of numerous different tissues both in vitro and in vivo.” Pluripotent refers to the ability of stem cells to turn into numerous different types of cells.
However, several challenges remain. Among them are the ethical issues associated with the use of embryonic stem cells, and the risk of provoking an immune response through stem cells created from donor tissue. The use of autologous stem cells (from the host’s own body) could be an alternative, since “[t]hese issues are circumvented when pluripotent cells are generated directly from the patient’s own somatic cells using the Yamanaka factors,” the authors said. Yamanaka factors include “transcription factors,” i.e., specific factors that researchers can access via gene therapy to program cells to become the specific type or types needed. These factors include Oct4, Sox2, Klf4 and c-Myc.
Unfortunately, the use of Yamanaka factors also carries some drawbacks. “A big challenge has been to increase the throughput [of] the reprogramming process, which generally is very low. Another disadvantage is the retroviral integration that is used in this method, due to the fact that this process comes with the risk of introducing mutations in the genome of the target cells,” the researchers said.
Introduced genetic mutations can potentially produce non-useable or even cancerous stem cells. To realize the full potential of stem cell treatments for PD and other neurodegenerative diseases, scientists first need to overcome the current challenges associated with stem cells. According to Anja Pen, PhD, and the study’s first author, “continued intensive research will have to prove whether [stem cells] are going to fulfill the potential they are believed to have in treating them.”






