Molecular Mechanism at Root of Chain Leading Parkinson’s Identified
Boston University School of Medicine and Northeastern University researchers have proposed a molecular mechanism by which only certain mutations in human apoA-1 protein cause familial amyloidosis while others do not. The research paper, entitled “Structural Stability and Local Dynamics in Disease-Causing Mutants of Human Apolipoprotein A-I: What Makes the Protein Amyloidogenic?”, was published in the Journal of Molecular Biology.
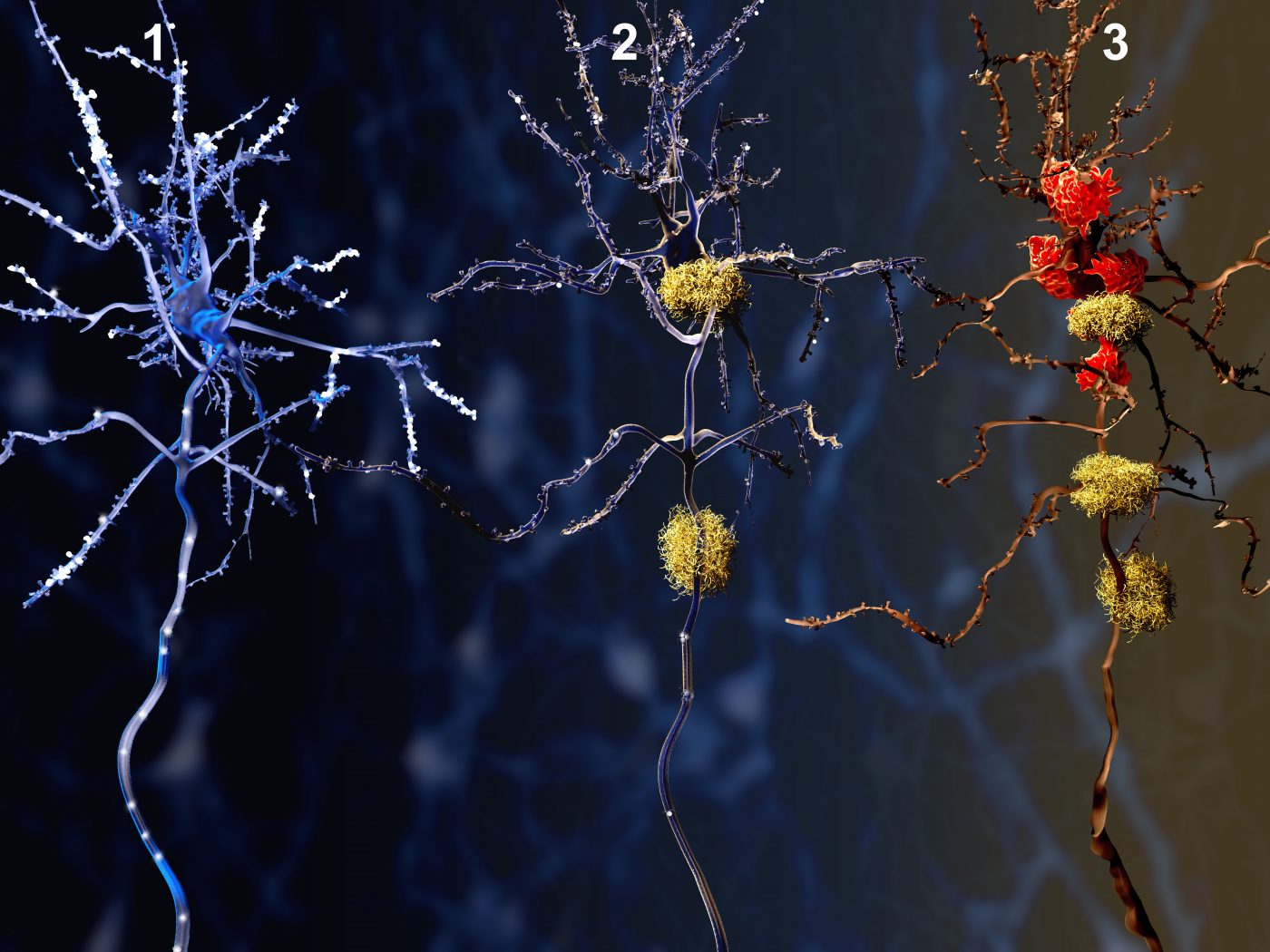
Alzheimer’s and Parkinson’s disease are included in the amyloidosis family of diseases, characterized by the abnormal deposit of insoluble protein aggregates, forming amyloid fibrils that damage organs and tissues. More than 26 proteins are currently known to potentially form amyloid aggregates.
One of the proteins forming amyloid fibrils is the apolipoprotein A-I (apoA-I), the major protein of plasma high-density lipoprotein (HDL), also known as the “good cholesterol” that removes cellular cholesterol and prevents atherosclerosis. In its normal form, the protein is essential to protect against cardiovascular disease. However, mutations or misfolding in the protein can cause familial amyloidosis, a potentially fatal condition where the protein forms aggregates in vital organs.
To understand the mechanism behind protein misfolding and why some mutations cause amyloidosis while others don’t, researchers analyzed the structure and stability of the human apoA-I and several natural occurring mutant forms. Results, from diverse molecular and structural techniques, revealed that a major amyloid vulnerable “hot spot,” thought to cause disease, does not always lead to amyloidoisis. Furthermore, mutations at one end of the protein were found to have a structural and functional effect in other parts of the protein. Certain mutations led to clearance of protein clumps instead of amyloid disease in humans.
According to a press release, the researchers suggest this finding is not limited to apoA-I but possibly applies to other amyloid-forming proteins, and may have important implications for potential treatments. Dr. Olga Gursky, professor of Physiology and Biophysics at BUSM and corresponding author of the study, commented, “If one could predict what makes any given protein to form amyloid, one could begin to design tools to decelerate or even block this pathogenic process before it starts.”






