Astrocytes Play a Role in Neurodegenerative Diseases
Written by |
Researchers at Trinity College Dublin, Ireland, discovered that specific cells in the brain called astrocytes develop an exaggerated reaction to inflammation in the context of neurodegenerative diseases. The study was recently published in The Journal of Neuroscience and is entitled “Astrocytes Are Primed by Chronic Neurodegeneration to Produce Exaggerated Chemokine and Cell Infiltration Responses to Acute Stimulation with the Cytokines IL-1β and TNF-alpha”.
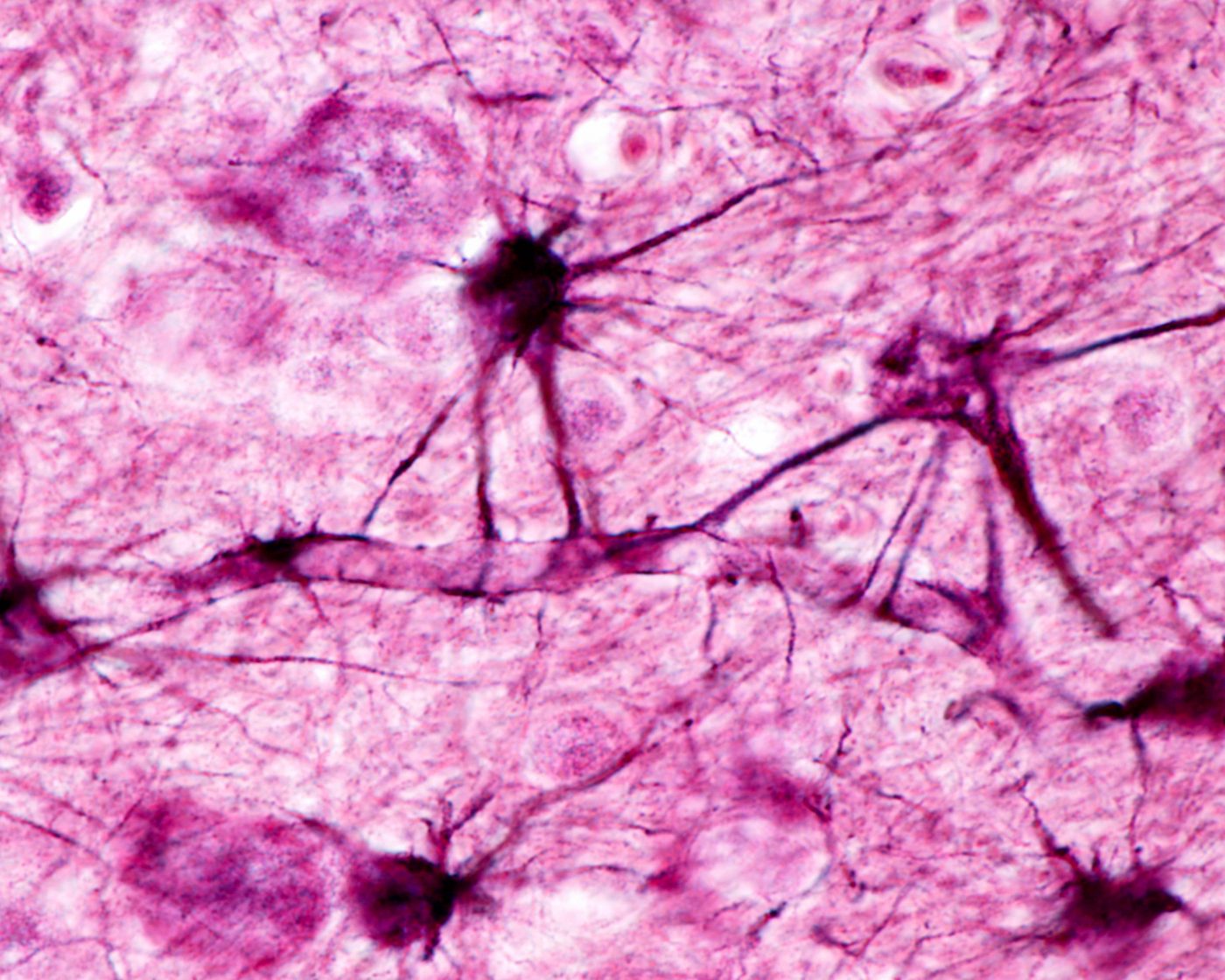
Astrocytes are cells critical for nutrient provision to the nervous tissue, maintenance of ion homeostasis and repair mechanisms in the brain and spinal cord. In the study, researchers hypothesized that astrocytes could also be involved in the response to inflammation.
Upon an acute injury to the brain or during neurodegeneration, astrocytes are stimulated, via inflammatory mechanisms, to produce chemokines, such as CCL2 and CXCL1, which are molecules that can recruit massive numbers of inflammatory cells from the periphery to the brain. In a young, healthy brain, this process is usually tightly regulated.
Using mice models with existing neurodegeneration and normal healthy animals, researchers have now discovered that astrocytes in neurodegenerating brains produce exaggerated levels of chemokines, leading to a large, uncontrolled infiltration of key immune cells like T cells, neutrophils and monocytes that can ultimately have extremely deleterious effects on the vulnerable brain.
Researchers suggest that astrocytes do play an important role in the inflammatory hypersensitivity of the degenerating brain, as they respond in an inappropriate and exaggerated manner in the presence of inflammatory stimuli. These findings are relevant for neurodegenerative conditions like Parkinson’s disease, a progressive neurodegenerative disorder that develops gradually with a worsening of the symptoms, from a barely noticeable tremor in the hands to serious difficulties in speaking, locomotion, coordination and balance. There is currently no cure for Parkinson’s, and it is estimated that four to six million people worldwide suffer from the disease.
The team believes that their findings increase the knowledge regarding the inflammatory vulnerability of the ageing and degenerating brain and suggest that therapeutic strategies should aim to decrease such susceptibility.
“If one recognizes the mechanisms by which the brain becomes susceptible to the effects of co-morbidities and environmental insults, one can then lessen their effects, irrespective of whether these strategies target the primary pathology. It is possible that targeting chemokines, or the inflammatory cells that produce them, may have protective effects in vulnerable patients.” concluded study’s senior author Dr. Colm Cunningham in a news release.





