Diagnosing Early Parkinson’s Disease With Gland Biopsy Shows Real Promise
Written by |
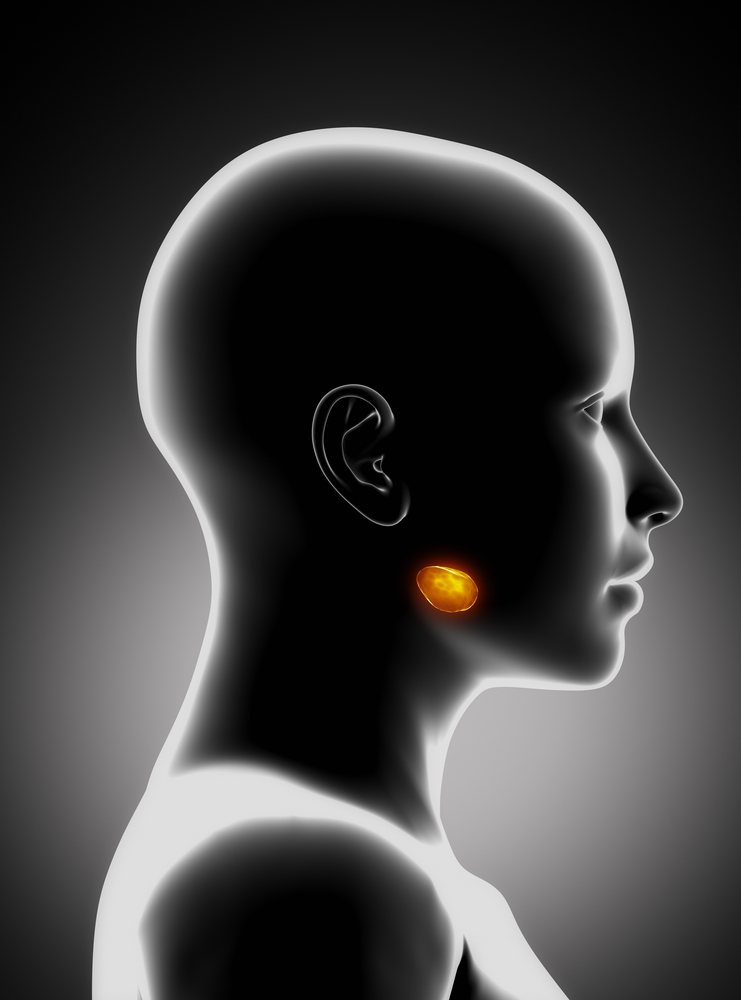
Mayo Clinic researchers in Arizona and Banner Sun Health Research Institute have found that a biopsy of a portion of a person’s submandibular gland may be a feasible approach to diagnose early Parkinson’s disease. The research is published in the journal Movement Disorders and titled “Peripheral Synucleinopathy in Early Parkinson’s Disease: Submandibular Gland Needle Biopsy Findings.”
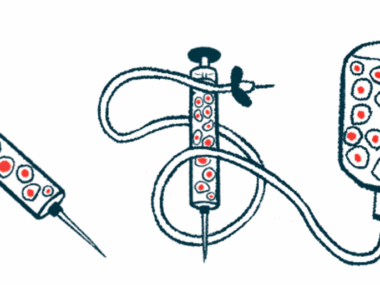
There has been great interest in the potential development of a peripheral tissue biopsy site for the diagnosis of Parkinson’s disease (PD); but there is currently no precise diagnostic test for the disease. Transcutaneous submandibular gland biopsy may provide the necessary accuracy. The test involves inserting a needle into the submandibular gland under the jaw to get to the core of the gland tissue within.
“This is the first study demonstrating the value of testing a portion of the submandibular gland to diagnose a living person with early Parkinson’s disease. Making a better diagnosis in living patients is a big step forward in our effort to understand and better treat patients,” said study author and neurologist Charles Adler, M.D., Ph.D., a professor of neurology at Mayo Clinic in Arizona, in a new release.
To determine whether needle biopsy of the submandibular gland reveals a protein known as Lewy type alpha-synucleinopathy in early Parkinson’s disease, 25 early Parkinson’s patients (those who had the disease less than five years) and 10 controls underwent transcutaneous needle core biopsies of the submandibular gland. Tissue was stained for phosphorylated alpha-synuclein, reviewed blind to clinical diagnosis, and only nerve element staining was considered positive.
“This procedure will provide a much more accurate diagnosis of Parkinson’s disease than what is now available,” said Thomas Beach, M.D., Ph.D., a neuropathologist with Banner Sun Health Research Institute. “One of the greatest potential impacts of this finding is on clinical trials, as at the present time some patients entered into Parkinson’s clinical trials do not necessarily have Parkinson’s disease and this is a big impediment to testing new therapies.”
The abnormal Parkinson’s protein was identified in 14 of the 19 patients who had enough tissue to conduct the analysis, providing data that will require further analysis to clarify the results. The team had previously determined that this biopsy could identify the protein in nine of 12 patients with an advanced stage of the disease. “This study provides the first direct evidence for the use of submandibular gland biopsies as a diagnostic test for living patients with early Parkinson’s disease,” Adler said. “This finding, in patients with early Parkinson’s disease, may be of great use since accuracy of diagnosis in patients with early disease is not nearly as good as in those having the disease for more than 10 years.”
According to the researchers, submandibular gland biopsy may also prove useful as a new gold standard, short of autopsy, for validation of other candidate biomarkers, although further data on this procedure is necessary.