Parkinson’s Studies May One Day Turn on Mouse-Human Chimeras
Written by |
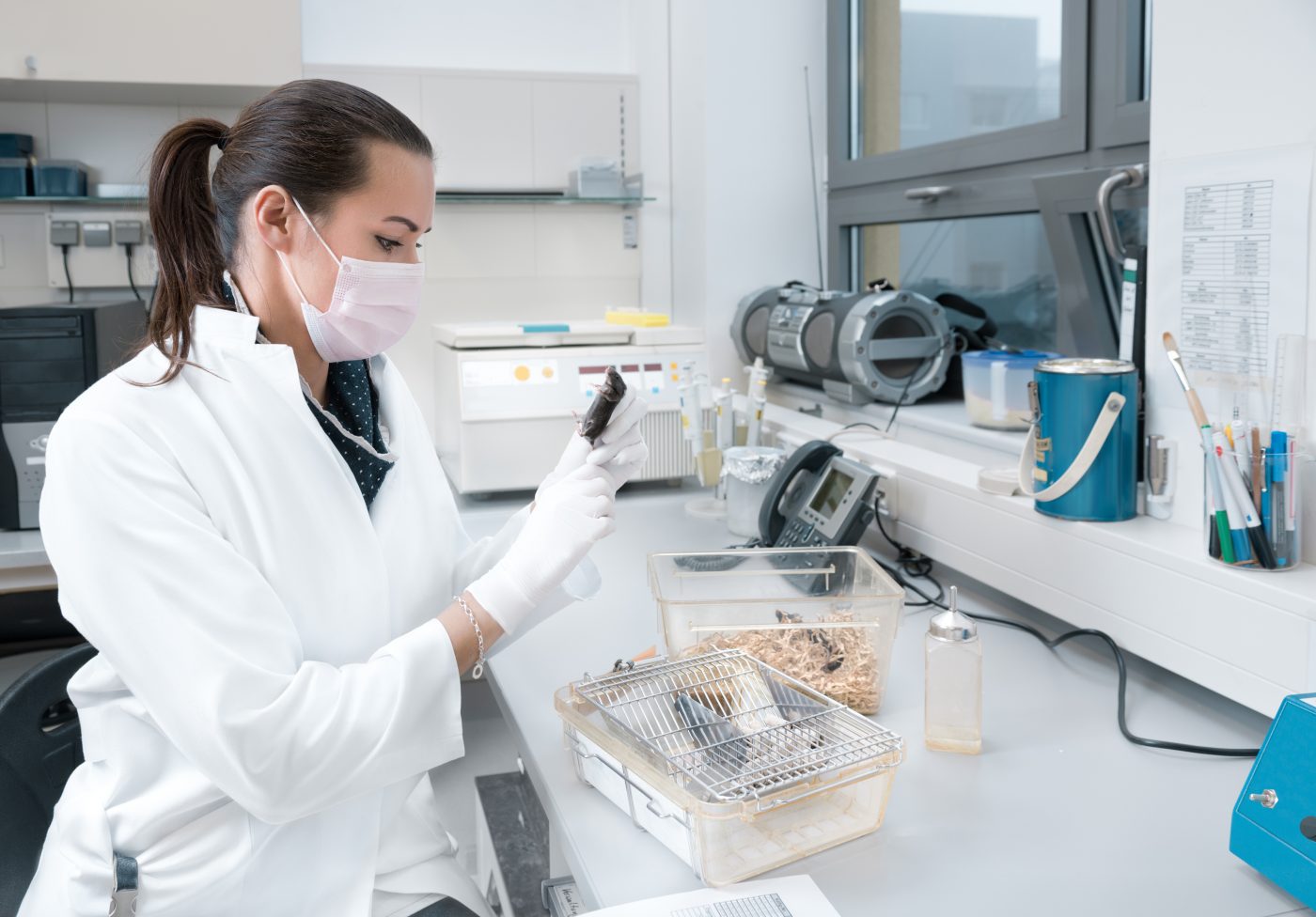
Researchers at the Whitehead Institute have created a promising mouse model to study embryonic development, and one that has the potential to serve as a model for neurological diseases such as Parkinson’s and cancers such as melanoma. The study describes the engineering and development of the mouse-human chimera, or mice born carrying human cells.
The article, “Human neural crest cells contribute to coat pigmentation in interspecies chimeras after in utero injection into mouse embryos,” appeared in Proceedings of the National Academy of Sciences (PNAS).
Researchers, led by Dr. Malkiel Cohen, developed the mouse-human chimera model by injecting neural crest cells (NCCs), derived from human embryonic stem cells (hESCs) and human pluripotent stem cells (iPSCs), into mouse embryos in utero. This way, scientists expected that human NCCs would integrate and differentiate into the host mice. NCCs, multipotent cells, can give rise to peripheral nervous system cells, and to cells that produce the pigment found in the skin and hair (melanocytes).
Implanted NCCs, labeled with the fluorescent protein GFP to track their movements, had a similar migration pattern to that exhibited by “natural” NCCs during development. Observations showed that about 27 percent of the implanted embryos had GFP-labeled NCCs present during development, a similar rate observed in the parallel construction of mouse-mouse chimera models. Moreover, about 35 percent of the live mice showed successful NCCs integration and differentiation into the host.
This model system, now being improved by the researchers, is a novel paradigm that might allow the study of development of human cells in in vivo conditions. Furthermore, this platform might allow a more personalized study of disease, by investigating human disease in mice using patient-derived iPSCs.
“The key barriers for human cells to functionally integrate into the mouse embryo are the significant differences in the biology of the human donor and the rodent host. Our next step will be to manipulate the mice and/or the injected human cells in order to allow better matching between the hosts and the donor human cells, hence to get better contribution by the cells successfully introduced into the embryo,” Dr. Cohen said in a press release.
Added Rudolf Jaenisch, the study’s first author, “The results are encouraging and provide a proof of principle — an important first step toward the goal of generating mice that carry disease-relevant human cells in the relevant tissue.”