Nanoparticle-based DNA Barcoding Could Be Used to Test Gene Therapies, Study Shows
Written by |
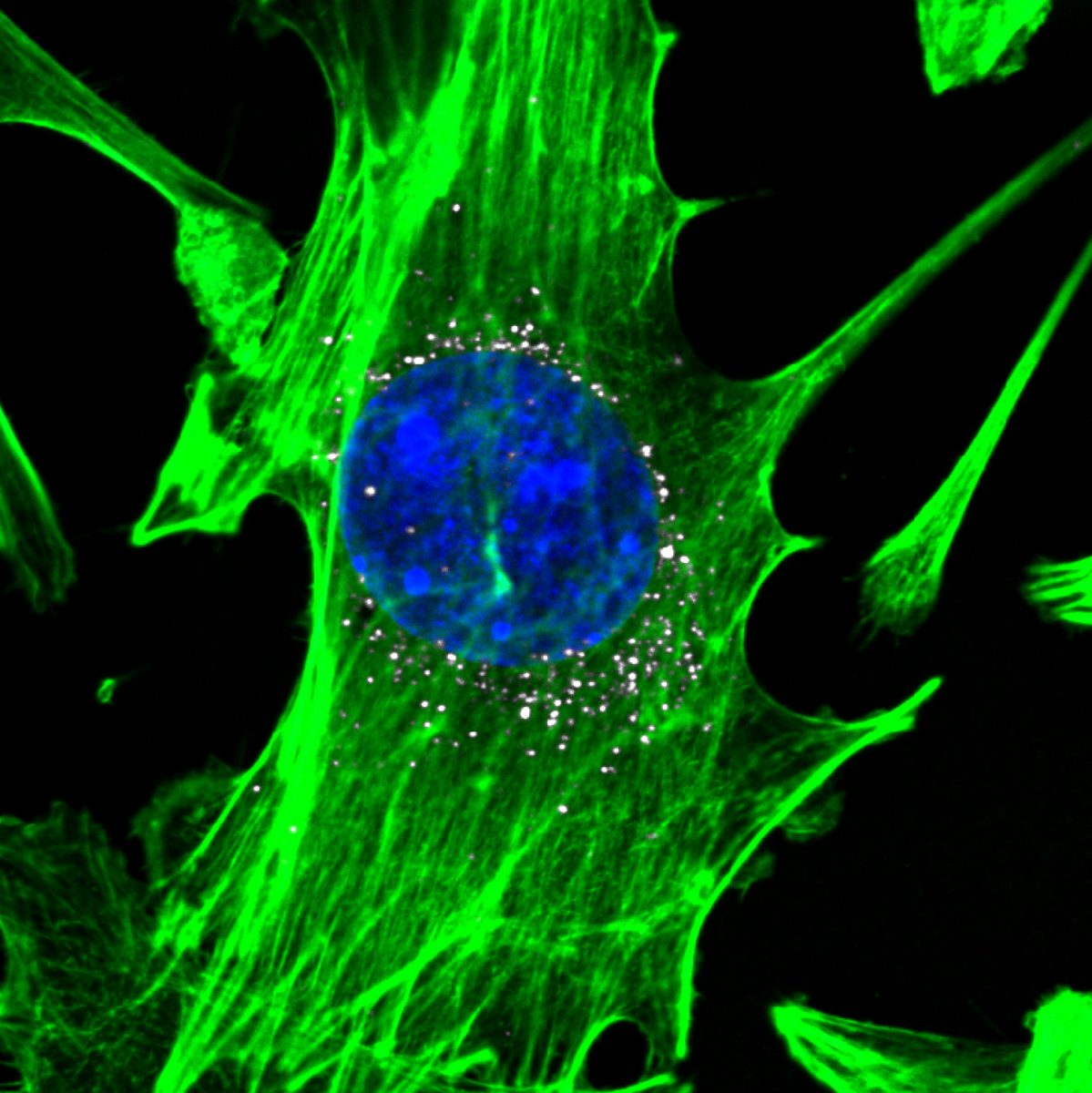
Cells, stained in green with blue nuclei, are targeted by nanoparticles carrying DNA barcodes (white). The nanoparticles efficiently delivery their DNA payload into the cells. (Image courtesy of Daryll A. Vanover, Kalina Paunovska, and Cory Sago at Georgia Tech).
A new DNA barcoding technique using nanoparticles could be used for large-scale testing of gene therapies for diseases such as Parkinson’s, according to Georgia Tech and Emory University researchers.
The study, “A direct comparison of in vitro and in vivo nucleic acid delivery mediated by hundreds of nanoparticles reveals a weak correlation,” appeared in the journal Nano Letters.
A well-known limitation of gene therapies is the difficulty of delivering DNA or RNA strands into the right cells. So far, scientists have relied on the standard method for studying nanoparticle delivery — lab dishes.
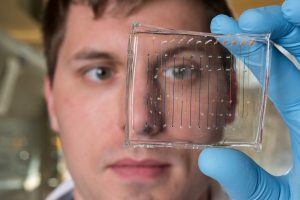
Researchers decided to look at a new technique. It involves attaching small snippets of DNA to different lipid-based nanoparticles, adding them to living cells in lab dishes, then injecting them into animals.
The team wanted to compare this new screening technique with the standard one, to see which was better.
They delivered 281 nanoparticles into endothelial cells and immune cells called macrophages. They discovered almost no correlation between how well the nanoparticles delivered the bar codes into cells in a lab dish or mice.
The researchers also studied how nanoparticle delivery can alter the microenvironment of certain tissue types. They found that cells derived from the same progenitor cells tend to be targeted by similar nanoparticles.
“If the in vitro [lab] tests had been good predictors, then particles that did well in the dish would also have done well in the animals, and particles that did poorly in the dish would also have done poorly in the animals. We did not see that at all,” James Dahlman, the study’s senior author, said in a Georgia Tech news release.
Importantly, this technique enables simultaneous testing of over 100 nanoparticles in a single animal. Using DNA sequencing methods, scientists are then able to discover which nanoparticles enter the cells of specific organs.
“If you wanted to test 200 nanoparticles in the traditional way, you would need 600 mice — three for each type of nanoparticle,” Dahlman said. “Using the DNA barcoding technique, which we call Joint Rapid DNA Analysis of Nanoparticles (JORDAN), we are able to do the testing in just three animals.”
The DNA strands used in the study are roughly the size of RNA-based molecules currently in development. Further work is necessary to determine whether the technique can use larger molecules.
The specificity of the new method is particularly important, as treatment of cancer or heart disease, for instance, requires precise targeting of diseased cells, while avoiding healthy tissues.
“These data demonstrate that barcoded lipid nanoparticles can elucidate fundamental questions about in vivo [animal] nanoparticle delivery,” the researchers wrote.
“DNA barcoding has the potential to advance the science of selecting nanoparticles for delivering gene therapies,” Dahlman said. “Using this technique, companies and academic labs could pick out promising nanoparticles much more efficiently. That could accelerate the rate at which nanoparticle-based therapies move into the clinic [clinical trials], while reducing the amount of animal testing required.”
Once promising nanoparticles are identified, scientists can then check their ability to deliver therapies. Only nontoxic nanoparticles can be screened, and inflammation generated by inserted DNA must be controlled.
“We hope this technique will be used widely in the field, and that it will ultimately bring more clarity to how these drugs affect cells — and how we can get them to the right locations in the body,” Dahlman said.
The research was supported by the National Institutes of Health, the Cancer Research Institute, Cystic Fibrosis Foundation, and Parkinson’s Disease Foundation.