Gene Therapy Preserves Nerve Fibers in Mouse Model of Severe Neurodegeneration
Written by |
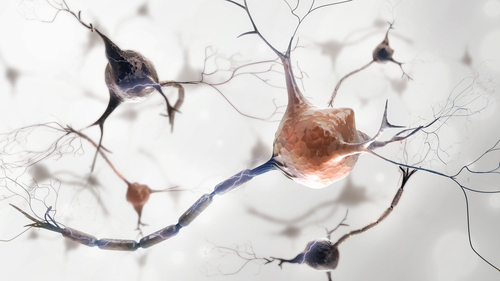
An investigational gene therapy was able to preserve nerve axons — long projections that connect nerve cells and transport information — in a mouse model of severe axonal degeneration.
Because axon degeneration precedes the death of neurons in several neurodegenerative diseases, including Parkinson’s disease and amyotrophic lateral sclerosis (ALS), the findings support this therapy’s potential as an effective treatment.
The study, “Gene therapy targeting SARM1 blocks pathological axon degeneration in mice,” was published in the Journal of Experimental Medicine.
Axons, or nerve fibers, are the long projections of a nerve cell, which conduct electrical impulses away from the cell body to other nerve cells, muscles, and glands. There is currently no treatment that effectively inhibits axon degeneration.
When an axon is injured, a protein called SARM1 becomes activated and triggers axons to self-destruct. In healthy nerve cells, this protein is switched off. Deleting the gene that codes for this protein, the SARM1 gene, has been shown to have a protective effect against axonal degeneration after injury in both a fruit fly model and a mouse model.
SARM1 acts as an enzyme that destroys metabolic factors needed for axons to work properly. It works by rapidly degrading a metabolite, called NAD+, causing a metabolic failure in neurons that trigger axonal degeneration. When this protein is mutated, it prevents rapid energy loss and subsequent destruction of axons.
SARM1’s multiple components must bind together for the protein to work properly. If one of these components is changed, the protein’s assemblage is faulty and unable to function. As such, scientists only have to alter or mutate a part of the protein to inhibit its function.
Researchers at St. Louis’ Washington University School of Medicine have developed a gene therapy to block the activity of SARM1.
The team introduced single mutations, affecting only one nucleotide — the building blocks of DNA — in the SARM1 gene, which resulted in the production of a faulty SARM1 protein. Similar to neurons without the SARM1 gene, when this gene therapy was inserted into nerve cells grown in the laboratory, no axonal degeneration was observed.
Accordingly, in injured neurons with a normal SARM1 protein, NAD+ levels were reduced. However, upon treatment with the gene therapy, they remained constant.
Researchers then treated neurons with vincristine, a chemotherapy agent, to simulate nerve cell damage. Two days later, the treatment resulted in axonal fragmentation. However, neurons that received the gene therapy remained intact and had normal metabolic activity — proof of how the therapy was able to inhibit SARM1 function.
To test the gene therapy in living organisms, the team used an inactive virus — adeno-associated virus (AAV) — as a vehicle to deliver the therapy into nerve cells of a mouse model of severe axonal degeneration. Researchers had induced a severe nerve injury in the sciatic nerve to trigger axonal degeneration.
Within five weeks, the viral vector containing the altered SARM1 gene was present in several of the affected nerves, including peripheral nerves and spinal cord nerve cells.
In animals treated with the gene therapy, their axons remained intact up to 10 days after nerve injury, and neurons preserved their normal conformation, architecture and myelin — a protective coating around nerve fibers — thickness.
In control (untreated) mice, there was almost a complete (99%) loss of axons at sites of nerve injury.
“With our viral gene therapy, we delivered a mutated form of SARM1 that is not only inactive itself but also blocks normal SARM1 proteins that have become activated in mice with nerve injuries,” senior author Jeffrey D. Milbrandt, MD, PhD, said in a university news release. “For a long time, viral gene therapy was a pipe dream, but there are now a number of ongoing clinical trials in other disorders that suggest we are on a promising track.”
“This has the potential to be transformative because it cuts across so many diseases,” said co-senior author Aaron DiAntonio, MD, PhD. “Rather than addressing a single disease, it is potentially a treatment for a disease process that is shared among many different neurodegenerative disorders.”


