Mitochondrial Interaction Networks May Help in Diagnosing Parkinson’s
Written by |
Networks of mitochondrial interactions in nerve cells may be used as a biomarker in diagnosing Parkinson’s disease, a recent study has shown.
The study, “Mitochondria interaction networks show altered topological patterns in Parkinson’s disease,” was published in the journal Nature Systems Biology and Applications.
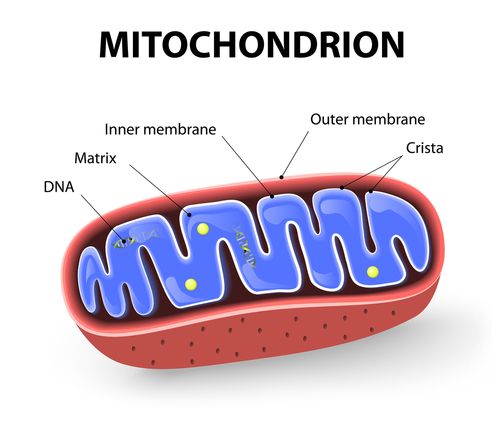
Mitochondria are small organelles within cells that produce energy needed for a wide range of physiological tasks. Old and/or damaged mitochondria can seriously damage cells, however, when not properly recycled.
“Since conventional analysis focusing on individual mitochondria has not provided satisfying insights into [Parkinson’s] pathogenesis, our pioneering work has gone a step forward by investigating the interaction networks between these organelles,” Feng He, PhD, the study’s principal investigator, said in a press release.
The researchers studied these interactions by comparing mitochondrial networks in the neurons of Parkinson’s patients to those of age- and sex-matched healthy controls.
They examined mitochondria in the ganglia — groups of sensory nerves — of the ascending and descending colon and of midbrain dopamine-producing (dopaminergic) neurons made from induced pluripotent stem cells (iPSCs). Of note, dopaminergic neurons are those that are gradually lost throughout the course of Parkinson’s disease.
The patients whose samples were studied had point mutations (changes in a single letter of the genetic code) in the SNCA (PARK1), RHOT1, and VPS35 (PARK17) genes, mutations which are implicated in the risk of developing Parkinson’s disease.
One patient had a SNCA triplication, meaning that they carried three copies of that gene, which is known to affect neuronal development.
The mitochondria of the colon ganglia formed larger sub-networks in Parkinson’s patients than in healthy controls. The investigators hypothesized that the increased size made these networks less efficient, perhaps slower to pass along energy or information to a given destination. This sort of delay might contribute to observable symptoms.
On the other hand, the researchers point out that such large and inefficient sub-networks could also play certain beneficial roles, such as buffering harmful signals.
Larger networks are typically built from recurrent smaller features — “building blocks” often referred to as motifs. The motifs forming mitochondrial networks in Parkinson’s patients also differed from those found in healthy controls.
The mitochondria in Parkinson’s-related motifs appeared to need to more fully interact with each other in order to maintain sufficient levels of cellular energy, than those of healthy controls, which require fewer interactions to transmit a given signal.
Visually, this is akin to one team in a soccer match needing each player to touch the ball on its way up the pitch, while the other team can pass it straight from defender to forward. The ball can cross the pitch either way, but one will take much longer.
The patterns seen in the mitochondrial interaction networks of people with Parkinson’s correlated with commonly-used clinical scores such as the Unified Parkinson’s Disease Rating Scale.
The investigators reasoned that if network features correlated with Parkinson’s scores, then they should also predict Parkinson’s disease.
A machine-learning algorithm — a computer procedure that makes predictions based on a set of inputs — accurately distinguished between Parkinson’s patients and healthy controls based solely on mitochondrial network features.
The researchers next compared these findings to lab-grown midbrain dopaminergic neurons derived from iPSCs of patients with sporadic (of unknown cause) and familial (of known genetic cause) Parkinson’s.
These cells showed the same mitochondrial network features as those of the colonic nerves.
To show that the network alterations in patients with familial Parkison’s were, in fact, caused by Parkinson’s-related mutations, the investigators “fixed” the SNCA point mutation with CRISPR/Cas9 gene editing tools, which significantly reversed the altered network patterns.
“Our findings bring forward the potential of using particular mitochondrial network features as novel biomarkers for the early diagnosis and classification of [Parkinson’s disease] patients, which might help develop a new health index,” Rejko Krüger, MD, one of the study’s authors, said.
“As a next step, we will explore how our results may offer new perspectives for the understanding of various other neurodegenerative diseases characterized by mitochondrial dysregulation, such as Huntington disease and Alzheimer’s, making our work a true instance of translational and transversal research,” he added.
Finally, the researchers note that although they tested their network analysis in mitochondria, the same approach can be applied to other organelles, such as endoplasmic reticulum and lysosomes.





