CST-103 Improves Brain Blood Flow in Early Clinical Trial
Written by |
Treatment with the investigational therapy CST-103 increased blood flow to certain regions of the brains of people with Parkinson’s disease and mild cognitive impairment, results of a small clinical trial show.
The type of increased blood flow that was seen “correlates with increased neuronal activity and cognitive benefit,” Gabriel Vargas, MD, PhD, said in a press release. Vargas is chief medical officer of CuraSen Therapeutics, which is developing CST-103.
According to CuraSen, people with Parkinson’s and other neurodegenerative diseases commonly have dysfunction in a region of the brain called the locus coeruleus.
Normally, the locus coeruleus is responsible for releasing signaling molecules that activate protein receptors called beta-2 adrenoceptors. The activation of these receptors is thought to promote a number of biological activities that help to keep brain cells healthy. This system of biochemical signals is called the noradrenergic system.
CST-103 is an agonist (activator) of beta-2 adrenoceptors. It is intended to restore the functionality of the faulty noradrenergic system in people with neurological diseases.
“Beta-2 agonists like CST-103 activate multiple cell types in the brain, leading to both maintenance of cognitive function and restoration of complex homeostatic pathways critical for protecting brain health,” said Anthony Ford, PhD, CuraSen’s CEO. “This approach represents an important step towards improving daily activities for millions of poorly managed patients, and offers a longer term option for limiting and potentially reversing pathological decline.”
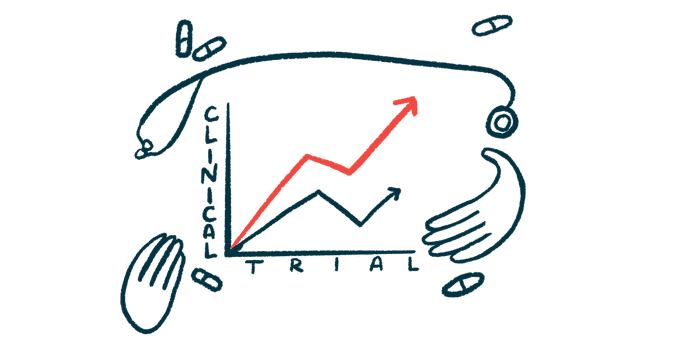
The new data come from a Phase 1 clinical trial that enrolled eight people with Parkinson’s or mild cognitive impairment (MCI), which is is the diagnosis when a person has notable cognitive and/or memory problems, but still can function independently in day-to-day life. Some people with MCI will go on to develop more serious forms of dementia, such as Alzheimer’s disease.
The eight trial participants were given a single 80 microgram (ug) dose of CST-103. Blood flow in their brains, sometimes called cerebral perfusion, was evaluated via MRI scan before taking the therapy, and again three hours after taking it.
Results showed that CST-103 significantly increased cerebral perfusion in several important regions of the brain, including the hippocampus (which is important for memory), the thalamus (which helps control movement and sensation) and the amygdala (an important regulator of emotion). In all regions, the average increase was more than 13%.
“By activating these excitatory adrenergic receptors with CST-103, we observed significant increases in cerebral perfusion in patients, especially in cognitively critical areas such as the hippocampus, thalamus and amygdala,” Vargas said.
He added that this increase in blood flow is likely indicative of increased brain cell activity in these regions. When these cells are more active, they need more energy, which they get from an increase in blood flow.
CST-103 generally was safe and well-tolerated, but when given on its own, it caused side-effects such as increased heart rate, tremor, and palpitations — known problems that arise when beta-2 adrenoceptor agonists are administered throughout the body.
After the first dose of CST-103 in the trial, participants underwent a week-long washout period. Then, all participants received another dose of the medication, with cerebral perfusion evaluated before and after. At this time, half of the patients also were given 1 mg of CST-107, which is an antagonist (blocker) of beta-2 adrenoceptors that, unlike CST-103, is not very good at getting into the brain.
Results showed that the co-administration of CST-103 and CST-107 “mostly eliminated” the side effects associated with CST-103 on its own, according to CuraSen.
The results “demonstrated that the common peripheral side effects of systemic administration of beta-2 agonists, such as increased heart rate, can be well managed by co-administering low doses of CST-107, a beta blocker, with CST-103,” Vargas said.
CuraSen is currently sponsoring a Phase 2 clinical trial (NCT04739423) to further evaluate the safety and efficacy of CST-103 plus CST-107. The trial is recruiting participants with Parkinson’s disease who have either dementia with cognitive fluctuations, or REM sleep behavior disorder (RBD) and symptoms of depression. It also is open to patients with MCI and depression, or Lewy Body Dementia with cognitive fluctuations.
The study is actively enrolling at locations in Australia, New Zealand, and the U.K. CuraSen also is planning to launch another trial to test CST-103 plus CST-107 in people with Parkinson’s who have gait freezing — when patients feel as if their feet are “glued” to the floor and can’t move forward.
CuraSen also is planning another trial early next year to test CST-2032, another beta-2 adrenoceptor agonist, in people with Parkinson’s or Alzheimer’s.
“CST-103 and potentially other proprietary beta-2 adrenergic agonists in the CuraSen pipeline offer a promising new strategy to improve cognitive deficits resulting from neurodegenerative disease,” Ford said.