CRISPR/Cas9 Used to Bring LRRK2 Mutation to Possible Monkey Disease Model
Written by |
Using CRISPR/Cas9 gene editing tools, researchers introduced a common Parkinson’s disease mutation into stems cells of the marmoset monkey for a first time, paving the way toward a primate model of this disease.
They also showed that this common leucine-rich repeat kinase 2 (LRRK2) gene mutation behaves the same in marmoset cells as it does in human cells.
The study, “In Vitro CRISPR/Cas9-Directed Gene Editing to Model LRRK2 G2019S Parkinson’s Disease in Common Marmosets,” was published in Scientific Reports.
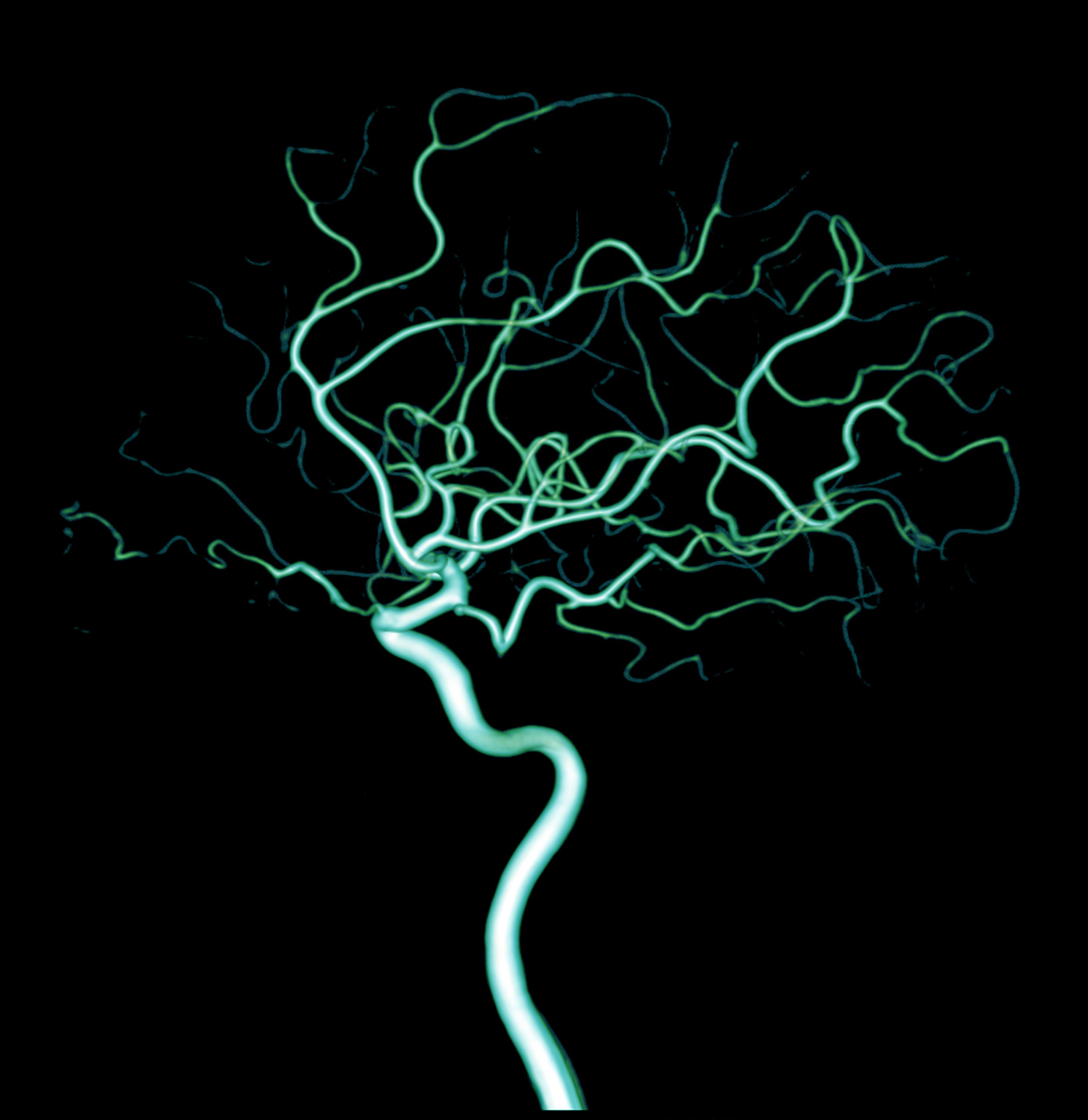
Parkinson’s, a progressive neurodegenerative disorder, results from the death of neurons that produce dopamine (dopaminergic neurons), a neurotransmitter needed to coordinate muscle movement. Loss of dopamine causes many of the disease’s observed symptoms, such as tremors, loss of balance, and slowed movements.
LRRK2 codes for an enzyme called dardarin, which plays an important role in cellular metabolism, such as autophagy (the cell’s recycling and waste-disposal system), and mitochondrial activity (the mitochondria function somewhat like a cell’s powerhouse).
Roughly 10% of Parkinson’s cases involve genetic mutations, and LRRK2 is the most commonly involved gene. Of those, 1% to 3% have a specific mutation in LRRK2 called G2019S. This mutation is thought to keep LRRK2 in its active form longer, allowing it to run amok inside cells.
Researchers at the University of Wisconsin-Madison created LRRK2 mutants in both embryonic and induced pluripotent stem cells (ESCs and iPSCs, respectively). They allowed these cells to grow into mature neurons, to compare the growth characteristics of all cells.
Of note, while ESCs are derived from early stage embryos (blastocysts), iPSCs are derived from either adult skin or blood cells that have been reprogrammed back into a stem cell-like state. This allows for the development of an unlimited source of almost any type of human cell needed for therapeutic purposes.
These mutated stem cells grew into the appropriate types of neural cells that are most affected during disease progression (dopaminergic neurons of the midbrain), but they did so less efficiently than healthy cells. They also grew fewer branches, which are needed to make and maintain connections with other neurons.
The mutated marmoset stem cells showed many features similar to patient-derived cells. Namely, they exhibited less autophagy and more reactive oxygen species (ROS), showed signs of mitochondrial dysfunction, and died more quickly than did their healthy counterparts.
An imbalance between the production of ROS and the ability of cells to detoxify them causes a biological phenomenon known as oxidative stress, which results in cellular damage and cell death.
Consistent with suggestions that LRRK2 remains active for longer than is healthy, the mutated cells showed increased markers of LRRK2 activity, despite containing overall less LRRK2 protein than non-mutated, or wild-type, cells.
As a further experiment, the researchers tested a potential genetic treatment for stopping LRRK2 hyperactivity. Chemical treatments have been developed to target the part of LRRK2 that is needed for its disease-causing effect, called the kinase domain. These kinase inhibitors, however, are associated with harmful side effects in the lungs of other animal models.
“We found no differences in viability between the cells with the truncated kinase and normal cells, which is a big thing,” Marina Emborg, a professor of medical physics and leader of the research team, said in a university news release. “And when we made neurons from these cells, we actually found an increased number of branches. This kinase gene target is a good candidate to explore as a potential Parkinson’s therapy.”
The researchers speculate that their new technique makes the marmoset a valid candidate species for a nonhuman primate Parkinson’s model.
Such models are vital, they wrote, “to the discovery of biomarkers and early intervention strategies aimed at halting or reversing the disease course.”


