8 or More Years of Contact Sports Linked to Parkinson’s-like Symptoms in Study
Written by |
Athletes playing contact sports for longer than eight years are six times more likely to develop Lewy body disease — a neurodegenerative disorder causing Parkinson’s-like symptoms — compared to those playing football, ice hockey or boxing for fewer years, a study reports.
Its authors suggest that years of continual injury to the brain, rather than those causing concussions, might be a determining factor.
The study, “Lewy Body Pathology and Chronic Traumatic Encephalopathy Associated With Contact Sports,” was published in the Journal of Neuropathology & Experimental Neurology.
Mild traumatic brain injuries (TBI), like concussions, that occur during contact sports are a growing health concern.
Playing contact sports for multiple years — regardless of concussion history — is already associated with brain imaging abnormalities. Consequently, players are considered to be at an increased risk of developing neurodegenerative diseases such as chronic traumatic encephalopathy (CTE), amyotrophic lateral sclerosis, Parkinson’s, and parkinsonism.
CTE develops as a result of repetitive head impacts, mainly through contact sports, and is characterized by abnormal changes in behavioral, mood, and cognitive and motor skills.
A 2016 study found an association between TBIs resulting in a loss of consciousness in people under age 25 and an increased risk of Lewy bodies — which correspond to aggregates of α-synuclein — in the brain.
Deposits of α-synuclein, called Lewy body disease (LBD), is associated with cognitive and motor abnormalities, and linked to later possible dementia and Parkinson’s disease.
Both trauma and CTE are also known to influence α-synuclein deposition in the brain, which can explain the motor symptoms sometimes found in athletes with chronic traumatic encephalopathy.
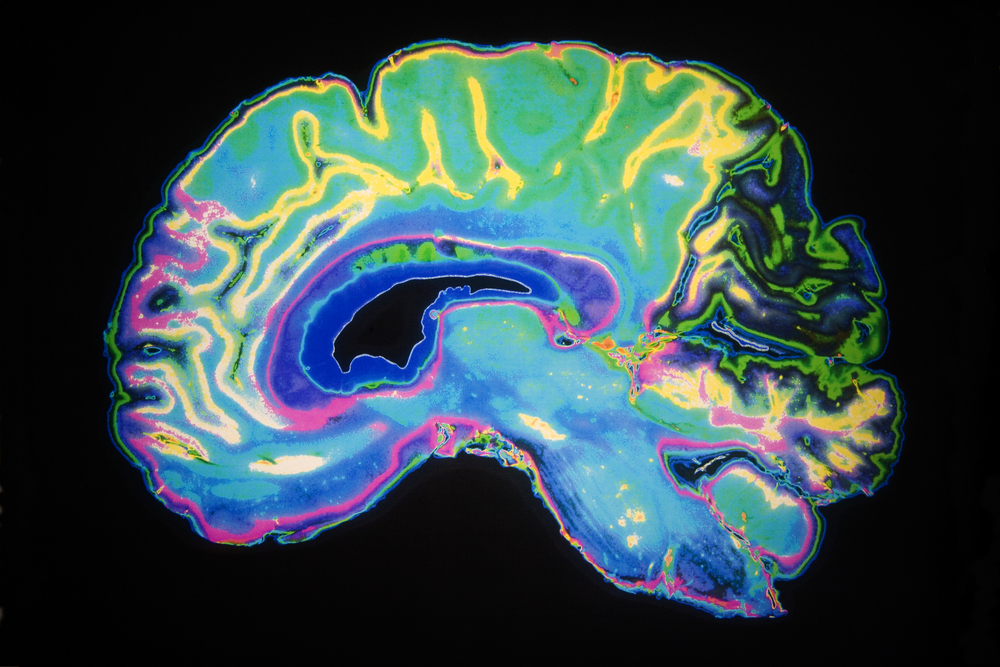
Researchers with Boston institutes examined whether contact sports and CTE are also linked with Lewy body disease. They assessed the presence and distribution of Lewy bodies in the brains of 269 deceased contact sports athletes (professional or amateur), 164 brain donations representing the community, and 261 from brain bank at the Boston University Alzheimer Disease Center.
The Parkinson’s Disease News Today forums are a place to connect with other patients, share tips and talk about the latest research. Check them out today!
The athletes had participated in sports that included American and European football, ice hockey, boxing, rugby, and the martial arts.
Contrary to what researchers expected, the regional distribution of Lewy bodies in the brains of CTE patients was similar to that seen in those with LBD.
Contact sports athletes were 1.3-fold more likely to develop neocortical LBD for each year they played. Neocortical LBD refers to deposition of Lewy bodies in the brain’s neocortex, the area responsible for such higher-order functions as cognition and motor commands.
A pooled analysis also showed that people who played contacts sports for more than eight years were the most likely to develop of neocortical LBD.
In fact, athletes in contact sports for more than eight years were 6.24-fold more likely to develop neocortical LBD compared to those playing in them for eight or fewer years, even after adjusting for possible confounding factors.
“The number of years of play of contact sports, not concussion history, best predicts CTE stage and the severity of tau pathology in the frontal cortex,” the study states.
Researchers also found that the presence of neocortical LBD, CTE stage, and Alzheimer’s disease were all significantly associated with dementia.
But parkinsonism (a Parkinson’s-like movement disorder) was associated only with neocortical LBD – suggesting that Lewy body disease is likely responsible for the motor symptoms seen in CTE patients.
“We found the number of years an individual was exposed to contact sports, including football, ice hockey, and boxing, was associated with the development of neocortical LBD, and LBD, in turn, was associated with parkinsonism and dementia,” Thor Stein, MD, PhD, a study author, neuropathologist at VA Boston Healthcare System and assistant professor at Boston University School of Medicine (BUSM), said in a press release.


