Gut Inflammation May Increase Risk for Parkinson’s Disease, Review Study Suggests
Inflammation in the gut, a hallmark of autoimmune disorders such as inflammatory bowel disease, may contribute to an earlier risk of developing Parkinson’s disease (PD), according to a recent review of genetic, epidemiological and animal model studies.
The risk, however, is very small with only 3% to 5% of patients with IBD eventually getting a Parkinson’s diagnosis.
The review, ”Inflammatory Bowel Diseases and Parkinson’s Disease,” was published recently in the Journal of Parkinson’s Disease.
PD is characterized by a range of inflammatory processes in the brain, including the release of pro-inflammatory signaling molecules (cytokines) and infiltration of immune cells.
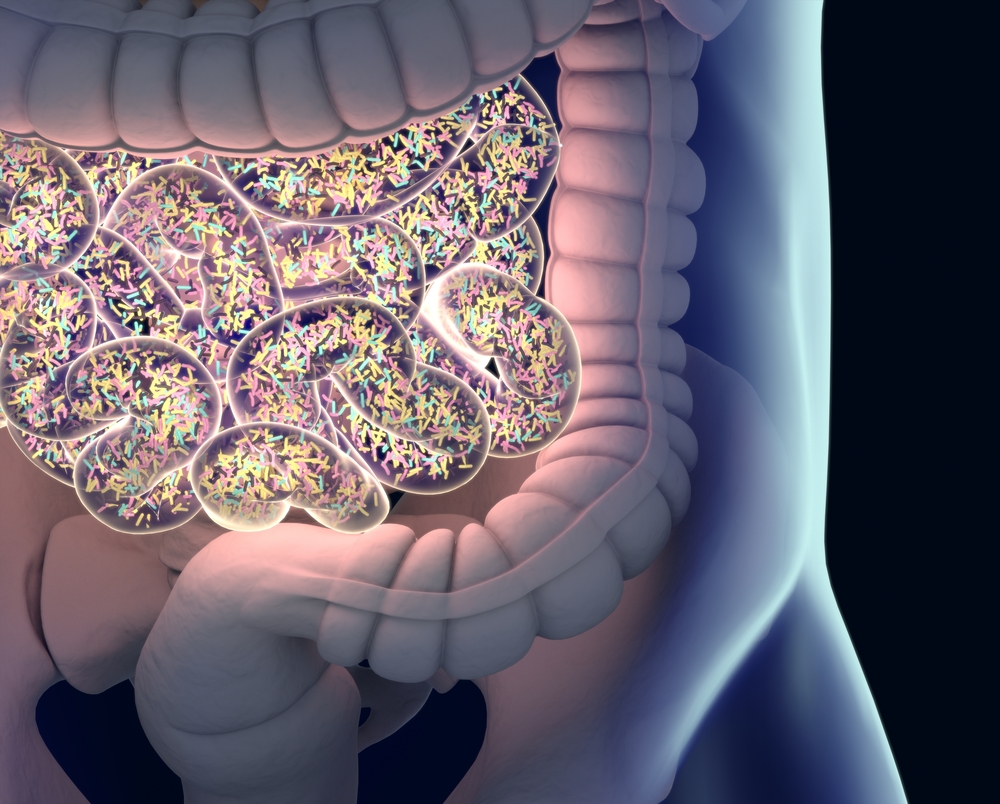
Increasing evidence, however, suggests that PD starts in the gastrointestinal system, with symptoms such as chronic constipation often emerging before motor symptoms develop.
“Experimental, clinical and epidemiological data suggest that intestinal inflammation contributes to the pathogenesis of PD,” the researchers wrote.
Gut infections are then thought to trigger alpha-synuclein release and subsequent aggregation, with the disease then spreading to the central nervous system (brain and spinal cord), where it promotes neurodegeneration. Alpha-synuclein is the protein that in PD becomes misfolded and forms toxic aggregates or clumps, which are the main component of Lewy bodies and greatly contribute to neurodegeneration.
“Parkinsonism is probably not just a brain disorder, but a group of diseases that may have their onset in the periphery, particularly in the gastrointestinal tract,” Tomasz Brudek, PhD, at the Copenhagen University Hospital and author of the review, said in a press release.
Inflammatory bowel disease (IBD) is triggered by prolonged inflammation of the digestive tract due to an imbalanced immune response. The two most common forms of IBD are ulcerative colitis and Chron’s disease.
Chronic inflammation of the gut is likely a predisposing factor for people to develop PD.
Genome-wide association studies (GWAS) have identified links between IBD and PD. Using GWAS, researchers analyzed the whole human genome searching for genetic changes associated with the disease. Mutations in the LRRK2 gene were found to be “a common susceptibility-factor” in both PD and Crohn’s disease, which may indicate a potential genetic link and common disease mechanisms.
An analysis of 138,511 genomes (our complete genetic “set”) from participants with European ancestry identified 17 genetic changes that occurred in both PD and autoimmune diseases, including ulcerative colitis and Crohn’s disease. Additional diseases included celiac disease, rheumatoid arthritis, type 1 diabetes, multiple sclerosis and psoriasis.
Several epidemiological studies also have shown a link between IBD and PD but with conflicting results. A meta-analysis of different population studies revealed that IBD patients had a 46% increased risk of having PD compared to controls. This association was still significant if ulcerative colitis and Chron’s disease patients were analyzed separately; those with Crohn’s had a 28% increased risk of PD, while those with ulcerative colitis had a 30% increased risk of PD when compared to healthy controls.
However, the authors noted that only a very small proportion of IBD patients will develop PD. “While IBD patients are more likely to get PD, the risk is still very small. For a given IBD patient, the probability of not getting the diagnosis is 95%–97%,” Brudek said.
The association of Parkinson’s disease with IBD may not be due to the disease specifically, but to gut inflammation in general.
“Inflammation of the gut is only one of many symptoms on the list of changes in the gut and is associated with neural structures in PD patients. Thus, IBD might be just one of many sources of intestinal inflammation,” Brudek said.
Animal studies have shown that inflammation in the gut can lead to the death of dopaminergic neurons — those that are mainly affected in Parkinson’s disease — supporting a link between gastrointestinal inflammation as a factor contributing to PD.
A recent study using a PD mouse model showed that alpha-synuclein aggregation occurred in the large intestine. This also was the case in wild-type (control) mice that were induced to develop colitis (inflammation of the gut).
When researchers induced colitis in the PD mouse model at a young age, they saw that mice went on to develop severe neurodegeneration later in life.
Several studies involving the post-mortem analysis of PD patients have reported the existence of alpha-synuclein aggregates in patients’ enteric nervous system (ENS) — the network of nerves that innervate the gastrointestinal tract — along with the brain.
Overall, these results support the existence of “connection between the intestinal environment and the CNS, [central nervous system], the so-called ‘gut-brain axis theory’ with a bi-dircetional communication between both,” Brudek wrote.
Similar to IBD patients, the gut microbiome — the natural community of microbes living in the gut — also is altered in people with PD, with an enrichment of a pro-inflammatory microbiome signature.
“Taken together, all data, including human, animal, and microbiome studies, suggest quite strongly that individuals with an increased tendency for peripheral inflammation have a higher risk to acquire PD. Given the potentially critical role of gut pathology in the pathogenesis of PD, there is reason to suspect that IBD may impact PD risk,” Brudek said.
Brudek proposed that future studies are required to identify risk factors associated with early (prodromal) PD that will support the development of therapeutic interventions for patients at higher risk of developing the disease.
Moreover, he added, it is important that clinicians recognize early the symptoms of PD in IBD, but also in patients with other chronic inflammatory disorders.
“We should direct our focus on the immune system in all Parkinsonian disorders, and further investigate the role of systemic inflammation and the immune system as such in these neurological diseases,” he said, adding that a “clear knowledge of the mechanisms implicated in gut/immune/nervous communication could help improve the prognostic and therapeutic tools leading to better quality of life for patients, reducing the exacerbation of PD symptoms, and delaying the progression of the disease.”






