Wireless Pacemaker-like Device May Offer Real-time Treatment for Parkinson’s, Study Reports
Written by |
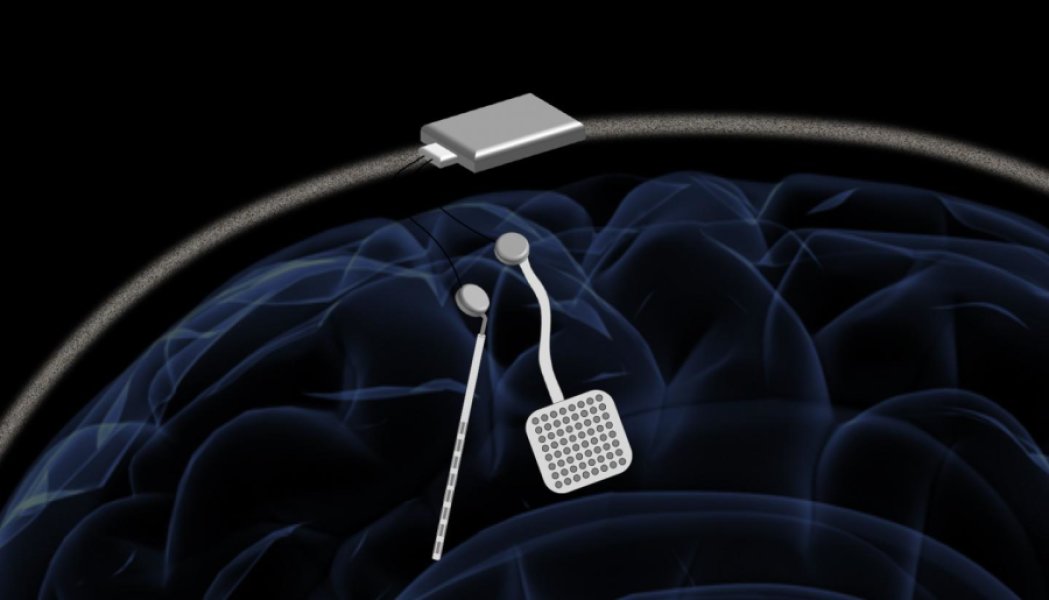
In a proposed device, two of the new chips would be embedded in a chassis located outside the head. Each chip could monitor electrical activity from 64 electrodes located into the brain while simultaneously delivering electrical stimulation to prevent unwanted seizures or tremors. Credit: Rikky Muller, UC Berkeley
A new neuromodulator — a wireless pacemaker-like device — may provide real-time treatment to patients with diseases such as Parkinson’s by monitoring abnormalities and delivering corrective electrical signals to the brain.
The device was described in the study, “A wireless and artefact-free 128-channel neuromodulation device for closed-loop stimulation and recording in non-human primates,” published in the journal Nature Biomedical Engineering.
Recent studies have shown that closed-loop neuromodulation systems could improve deep brain stimulation for treating Parkinson’s disease and other motor disorders. These systems deliver and adjust therapeutic electrical stimulation in response to a patient’s neural state in real time.
Up to this point, it has been difficult, both medically and economically, to apply closed-loop neuromodulation systems in patients with movement disorders, and it hasn’t been clear how to implement strategies for these treatments. Previous attempts were short term, using systems that were not fully implantable.
“In order to deliver closed-loop stimulation-based therapies, which is a big goal for people treating Parkinson’s and epilepsy and a variety of neurological disorders, it is very important to both perform neural recordings and stimulation simultaneously, which currently no single commercial device does,” study author Samantha Santacruz, PhD, now an assistant professor at the University of Texas, said in a press release.
Interested in Parkinson’s Disease research? Sign up for our forums and join the conversation!
To enable advanced research in closed-loop neuromodulation, “there is a need for a flexible research platform, for testing and implementing these various closed-loop paradigms, that is also wireless, compact, robust and safe,” the researchers wrote in the study.
The researchers, from the University of California, Berkeley and Cortera Neurotechnologies, introduce a new device in this study that allows simultaneous recording and stimulation of the brain. The WAND — wireless artifact-free neuromodulation device — is a miniaturized, autonomous neural interface capable of closed-loop sensing and stimulation while fully canceling stimulation artifacts — recorded electrical signals coming from the device. With this WAND, electrodes are surgically implanted inside the brain, with chips contained in a chassis attached to the outside of the head.
Existing devices can detect neural biomarkers — electrical signatures indicative of abnormal brain processes — and stimulate the brain in a closed-loop neuromodulation system, but they contain a low number of recording and stimulating channels. WAND improves on these limitations by incorporating a large number of recording and stimulation channels and a wireless data rate to support a large number of streaming channels. The technology also automatically adjusts stimulation parameters.
“The process of finding the right therapy for a patient is extremely costly and can take years. Significant reduction in both cost and duration can potentially lead to greatly improved outcomes and accessibility,” said Rikky Muller, PhD, an assistant professor of electrical engineering at University of California, Berkeley. “We want to enable the device to figure out what is the best way to stimulate for a given patient to give the best outcomes. And you can only do that by listening and recording the neural signatures.”
In a study of non-human primates, WAND enabled long-term recordings of local brain activity and the real-time cancellation of stimulation artifacts. The researchers proved that the closed-loop system device was causing changes in brain activity by using stimulation to create a functional change in the primates’ behavior during a routine task. To this end, the device enables neuroscientific discovery and preclinical investigations of stimulation-based therapeutic interventions.
“While delaying reaction time is something that has been demonstrated before, this is, to our knowledge, the first time that it has been demonstrated in a closed-loop system based on a neurological recording only,” Muller said. “In the future, we aim to incorporate learning into our closed-loop platform to build intelligent devices that can figure out how to best treat you, and remove the doctor from having to constantly intervene in this process.”





