Targeting Enzyme in Immune Cells of Brain May Slow Parkinson’s Progression, Study Suggests
Blocking the activity of an enzyme found in immune cells of the brain may prevent the degeneration and death of nerve cells seen in Parkinson’s disease, new research shows.
The study “Upregulation of HDAC2 in Laser Capture Nigral Microglia in Parkinson’s Disease,” was published in Neurobiology of Aging.
The enzyme being studied in this work, called HDAC2, regulates a critical cellular mechanism known as epigenetics. This is a mechanism that controls which genes are available to be read and translated into active proteins, and which genes are silenced and not available.
Because of its key role, HDAC2 — as well as other enzymes of its family — are seen as potential therapeutic targets for several neurodegenerative diseases. But the relevance of HDAC2 to Parkinson’s is not clear.
Arizona State University-Banner Neurodegenerative Disease Research Center researchers, along with collaborators at Jiao Tong University School of Medicine in China, analyzed the levels and activity of HDAC2 in brain tissue samples from Parkinson’s patients and healthy controls.
The team used an advanced technique called laser captured microdissection, which allows the selection and separation of specific cells within a tissue sample.
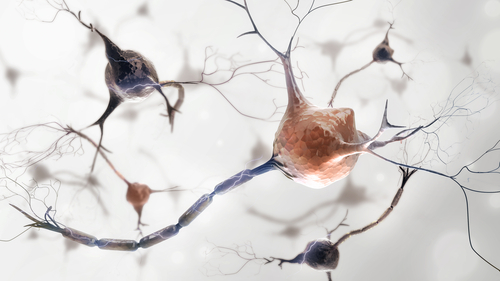
Brain immune cells, called microglia, and dopamine-producing nerve cells collected from Parkinson’s patient samples were found to have high levels of HDAC2 compared to the levels of these cells in healthy samples.
Interestingly, HDAC2 levels correlated with the amount of LN3 — a marker of microglia activity — in the Parkinson’s samples but not in the controls. This suggests that HDAC2 may be linked to the greater pro-inflammatory and abnormal (deregulated) activity of microglia, as they transition from protective brain cells to ones that attack and damage healthy neurons.
To further test this hypothesis, the team used experimental cell lines that reproduced the behavior of microglia, the brain’s resident immune cells, and were chemically pushed into a pro-inflammatory state.
These experimental cells showed increased levels of HDAC2, similar to the pattern found in Parkinson’s patients. However, this effect was only observed when cells were exposed to higher levels of the chemical activator, suggesting that brain’s immune cells “may have an inflammatory threshold that must be met” before significant differences in HDAC2 levels are achieved, researchers wrote.
“It has been known for some time now that within pro-inflammatory environments, like the substantia nigra in Parkinson’s disease, microglia are responsible for the constant upregulation and release of neurotoxic cytokines,” Diego Mastroeni, a study co-author and an assistant research professor in the ASU School of Life Sciences, said in a university news article.
These findings support HDAC2 as a specific target “that may be inhibited to reduce the expression of genes associated with neuroinflammation,” Mastroeni said. “The key will be targeting HDAC2 gene expression levels specifically in substantia nigra’s microglia.”






