Stem Cell Transplant Trial in Parkinson’s Patients Planned After Test in Japan Succeeds in Monkeys
Written by |
Researchers in Japan are preparing for a first human trial of induced pluripotent stem cells (iPSCs) in patients with Parkinson’s disease, after obtaining promising data from a study in monkeys.
The study, which appeared in the journal Nature, demonstrated that transplanting human iPSCs into the brains of the primate models of Parkinson’s was safe, and allowed the monkeys to move spontaneously.
Importantly, although researchers said the effectiveness could be compared to that of levodopa, the animals showed no signs of abnormal and jerky movements, known as dyskinesia.
Researchers from the Center for iPS Cell Research and Application (CiRA) at Kyoto University said the study, “Human iPS cell-derived dopaminergic neurons function in a primate Parkinson’s disease model,” made it clear that the technique was now close to being ready for assessment in humans.
They hope to launch a clinical trial by the end of 2018.
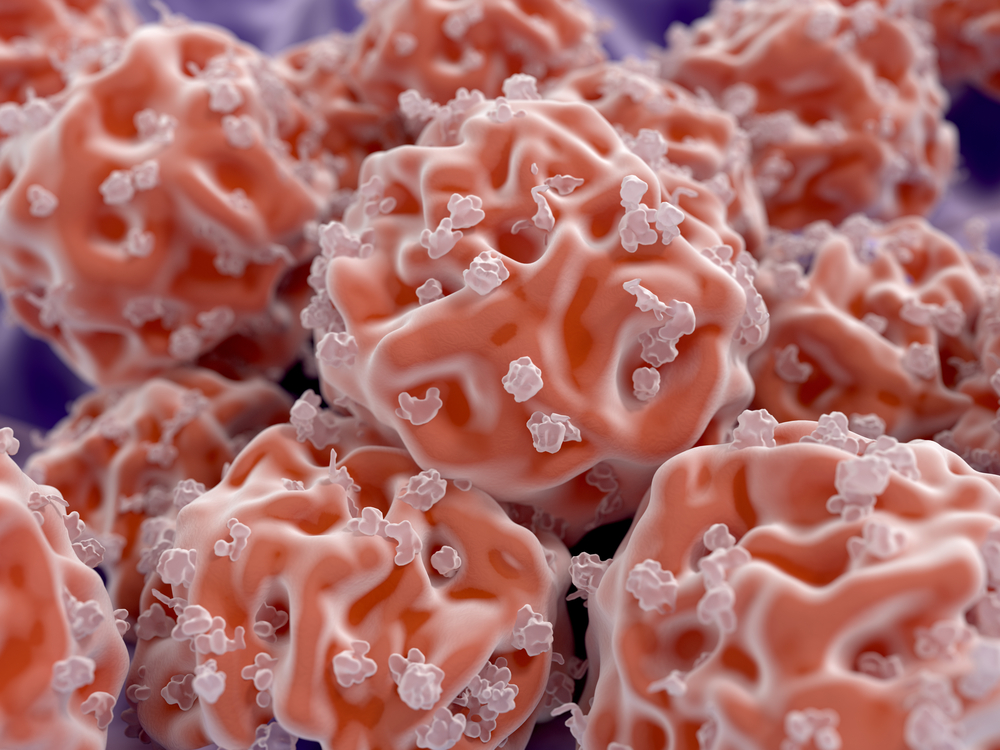
In contrast to embryonic stem cells, iPSCs are derived from adults. Researchers have learned how to backtrack a cell — most often from blood or skin — in its development to force it to become a stem cell. Such cells can then be grown into a range of specialized cells, including dopamine-producing neurons.
“Our research has shown that DA [dopamine] neurons made from iPS cells are just as good as DA neurons made from fetal midbrain,” Dr. Jun Takahashi, a professor and neurosurgeon specializing in Parkinson’s disease and the study’s senior author, said in a press release. “Because iPS cells are easy to obtain, we can standardize them to only use the best iPS cells for therapy.”
The Kyoto researchers made several key advances in their study in monkeys that had been exposed to a chemical that made the brain degenerate in a way similar to Parkinson’s.
They studied the animals for two years after the transplant and verified that the cells survived, and became integrated, forming new connections in the monkeys’ brains. Importantly, they showed that it was possible to track the health of the cells using brain imaging methods, such as magnetic resonance imaging (MRI) and positron emission tomography (PET).
This allows for a feasible way to monitor patients in clinical trials.
“MRI and PET are non-invasive imaging modalities. Following cell transplantation, we must regularly observe the patient. A non-invasive method is preferred,” Takahashi said.
But the work also demonstrated that cells from healthy donors did not outperform cells taken from Parkinson’s patients, and outcomes could be compared to tests with embryonic stem cells.
“We made DA neurons from different iPS cells lines. Some were made with iPS cells from healthy donors. Others were made from Parkinson’s disease patients,” said Tetsuhiro Kikuchi, a neurosurgeon working with Takahashi.
Researchers also underscored that the method used to grow neurons from iPSCs is suitable for clinical trials.
Using patient-derived cells is, from an immunological perspective, the best option, as the patient’s immune system will recognize they belong there once transplanted. But making individual cells for each patient is a far more costly and time-consuming procedure than making a batch of cells from a donor.
In a second study, “MHC matching improves engraftment of iPSC-derived neurons in non-human primates,” the team demonstrated that by matching donor cells to the patient with the help of immune markers, called MHC, the transplant elicited a lower immune response.
The publication in Nature Communications showed that monkeys given matched transplants required less immunosuppressive treatment to harness the immune response to a transplant, compared to those who received unmatched transplants.
“The combination of MHC-matching and immunosuppression will reduce the dose and duration of the immunosuppressive drug and be the best strategy for the transplantation,” said Asuka Morizane, a neurosurgeon and assistant professor at CiRA who lead the study.
The Nature study provided even further insights. Earlier, researchers believed that the number of transplanted cells was the most important factor to consider. But the team found the transplanted cells’ quality was a key factor for success.
“Each animal received cells prepared from a different iPS cell donor. We found the quality of donor cells had a large effect on the DA neuron survival,” Kikuchi said.
To assess cell quality, the team compared cells transplanted into monkeys with many surviving transplanted cells to those in which relatively few cells survived. A screen of gene activity provided researchers with a list of factors that stood out in the group with excellent outcomes.
One of these genes — called Dlk1 — has previously been identified as a marker of good outcomes in a study that assessed stem cell transplants in a rat model of Parkinson’s disease.
“Dlk1 is one of the predictive markers of cell quality for DA neurons made from embryonic stem cells and transplanted into rat. We found Dlk1 in DA neurons transplanted into monkey. We are investigating Dlk1 to evaluate the quality of the cells for clinical applications,” Kikuchi said.
Efforts using stem cell transplants to treat Parkinson’s are ongoing around the globe. One approach already being tested in a clinical trial uses so-called human parthenogenetic stem cells (hpSC).
These cells are derived from unfertilized egg-cells that are chemically stimulated to start dividing to form stem cells. According to International Stem Cell Corporation, which developed the treatment, these cells have the advantages of embryonic stem cells, but avoid the ethical dilemma, since they cannot generate a human being.
Yet others aim to use embryonic cells. Chinese and Australian research teams have already launched such studies, according to a Nature News article by Ewen Callaway, on the topic.
Although some researchers argue that there are issues to be resolved before stem cells can safely be tried in humans, the Japanese team appears confident of the feasibility of its approach.
“This study is our answer to bring iPS cells to clinical settings,” Takahashi said.


