Approved Blood Pressure Medication Also May Treat Parkinson’s Disease, Animal Study Suggests
Written by |
Felodipine, an approved therapy for high blood pressure, is able to promote the clearance of toxic protein aggregates in mouse models of neurodegenerative diseases, including Parkinson’s, according to a study.
The study, “Felodipine induces autophagy in mouse brains with pharmacokinetics amenable to repurposing,” was published in the journal Nature Communications.
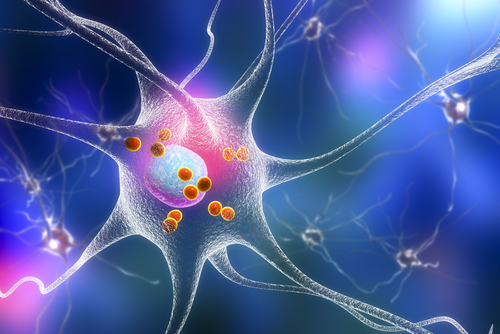
A common feature of most neurodegenerative diseases, such as Alzheimer’s, Parkinson’s, and Huntington’s diseases, is the accumulation of toxic protein aggregates within neurons, or brain cells. Buildup of these proteins damages the cells and leads to neurodegeneration in these disorders.
Toxic material is normally cleared from the body through a mechanism called autophagy, which refers to the process by which cells degrade and purge unwanted material, such as harmful protein clusters.
Because autophagy often is impaired in neurodegenerative diseases, researchers are interested in identifying chemical compounds that can stimulate this process and potentially improve the clearance of toxic aggregates and reduce disease symptoms. However, no such treatment exists yet.
One possibility is to identify an existing medication that can be used for this purpose. Therapeutic compounds frequently have multiple targets, which means the same therapy often can treat different conditions. It is typically easier and faster to repurpose existing therapies because they already have gone through clinical trials and been found safe for human use.
To try to find one of these medications that might induce autophagy and be suitable for treating neurodegenerative diseases, researchers at the UK Dementia Research Institute and the University of Cambridge screened several different therapies that were approved for other indications.
They previously had identified an approved medication for high blood pressure and angina known as verapamil (sold under the brand names Calan, Covera, and Verelan, among others) as a powerful inducer of autophagy. However, it does not cross the blood-brain barrier (a thin membrane that protects the central nervous system, including the brain) and is therefore not appropriate for the treatment of neurodegenerative diseases.
The researchers then screened a panel of similar therapies to identify any that actually would penetrate the blood-brain barrier and have strong autophagy-inducing effects. This led them to felodipine as the most suitable candidate.
Felodipine (sold under the brand name Plendil) is approved by the U.S. Food and Drug Administration for the treatment of hypertension (high blood pressure). Laboratory studies indicated that felodipine promotes autophagy and clears a variety of toxic protein aggregates found in neurodegenerative diseases.
To further investigate felodipine, researchers tested the effects of the compound in animal models of Huntington’s and Parkinson’s diseases.
They performed a pharmacokinetic analysis to determine the optimal treatment regimen in mice that would mimic the concentration the therapy reaches in humans at currently prescribed doses. (Pharmacokinetics refers to how a compound is absorbed, distributed, metabolized, and excreted in the body.)
Results indicated that felodipine was effective at reducing the buildup of aggregates in mice with the Huntington’s and Parkinson’s disease mutations, as well as in a zebrafish model of dementia. Furthermore, long-term treatment with felodipine was associated with a decrease in signs of the diseases.
Notably, these effects were observed at concentrations of felodipine that would be safe for humans.
“These data suggest that this drug may have efficacy in humans with appropriate neurodegenerative diseases that may be ameliorated by autophagy induction,” the authors wrote.
“This is the first time that we’re aware of that a study has shown that an approved drug can slow the build-up of harmful proteins in the brains of mice using doses aiming to mimic the concentrations of the drug seen in humans,” David Rubinsztein, PhD, said in a press release. Rubinsztein, a professor of molecular neurogenetics at Cambridge, led the study. “As a result, the drug was able to slow down progression of these potentially devastating conditions and so we believe it should be trialled in patients.
“This is only the first stage, though. The drug will need to be tested in patients to see if it has the same effects in humans as it does in mice. We need to be cautious, but I would like to say we can be cautiously optimistic,” he said.