Common Anti-inflammatory Medication May Help Prevent Parkinson’s Neurodegeneration, Study Suggests
A type of immune cell called Th17 may be a key a promoter of neurodegeneration in Parkinson’s disease by producing the pro-inflammatory molecule interleukin-17 (IL-17), according to a study.
Researchers also found that the common anti-inflammatory medication Cosentyx (secukinumab), an antibody against IL-17, seems to prevent this mechanism and the death of nerve cells.
The study, “Th17 Lymphocytes Induce Neuronal Cell Death in a Human iPSC-Based Model of Parkinson’s Disease,” appeared in the journal Cell Stem Cell.
Responses from the immune system are usually divided into two categories. Innate immune responses are part of the body’s first line of defense and are not specific to a particular pathogen. Adaptive immune responses, however, are specific to certain invaders or molecules, and use a “memory” to boost the response.
Abnormal regulation of T-cells during adaptive immune responses is well-known in chronic inflammatory autoimmune disorders such as multiple sclerosis.
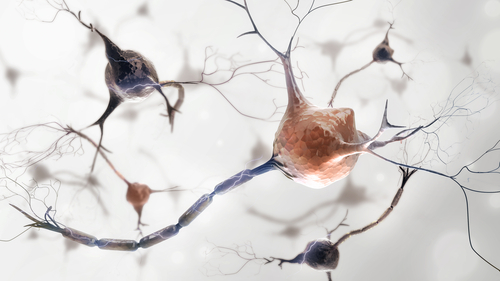
However, unlike the role of inflammation via innate immune cells, the contribution of the adaptive response to neurodegeneration in Parkinson’s — in particular the hallmark loss of dopamine-producing neurons in an area of the brain called substantia nigra — remains largely unexplored.
Studies have shown the presence of specific subsets of T-cells, as well as their activation, in the brains of Parkinson’s patients. Results from animal models also suggested that these cells are important in Parkinson’s, but scientists have been unable to prove that T-cells directly promote neurodegeneration in human neurons.
Join the Parkinson’s forums: an online community for people with Parkinson’s Disease.
Aiming to address this question, researchers at Friedrich-Alexander-Universität Erlangen-Nürnberg (FAU) in Germany collected skin samples from Parkinson’s patients and healthy individuals used as controls, which were used to create midbrain neurons — where the substantia nigra is located.
These cells were then cultured along with T-cells collected from the patients’ blood.
First, the scientists found that amounts of Th17, a type of T-cell implicated in inflammation, in the blood were associated with a greater neuron cell death in culture. This Th17-driven neurodegeneration was not observed in the control group.
The team then found that neuronal death was mediated by elevated amounts of the IL-17 pro-inflammatory protein — which is produced by Th17 cells — and activation of NFkB, a complex of proteins that regulate gene expression and have previously been associated with chronic inflammation and neurodegenerative diseases, among other disorders.
Importantly, blocking IL-17 or its receptor, or adding Cosentyx — an IL-17A antibody approved for the treatment of psoriasis, psoriatic arthritis, and ankylosing spondylitis — largely prevented neuronal death.
“Overall, our findings indicate a critical role for IL-17-producing T cells in human [Parkinson’s]-associated neuronal cell death,” the researchers wrote.
“Thanks to our investigations, we were able to clearly prove not only that T-cells are involved in causing Parkinson’s disease, but also what role they actually play,” Beate Winner, MD, a stem cell researcher at FAU, said in a press release. “The findings from our study offer a significant basis for new methods of treating Parkinson’s.”