Parkinson’s Patients on Dopamine Replacement Therapy Should Be Monitored for Psychosis, Study Suggests
Written by |
Psychosis is an important marker for impaired volition (the act of making a conscious choice) in people with Parkinson’s disease who are treated with dopamine replacement therapy, a new study shows.
The study, titled “Markers of impaired motor and cognitive volition in Parkinson’s disease: Correlates of dopamine dysregulation syndrome, impulse control disorder, and dyskinesias,” was published in the journal Parkinsonism and Related Disorders.
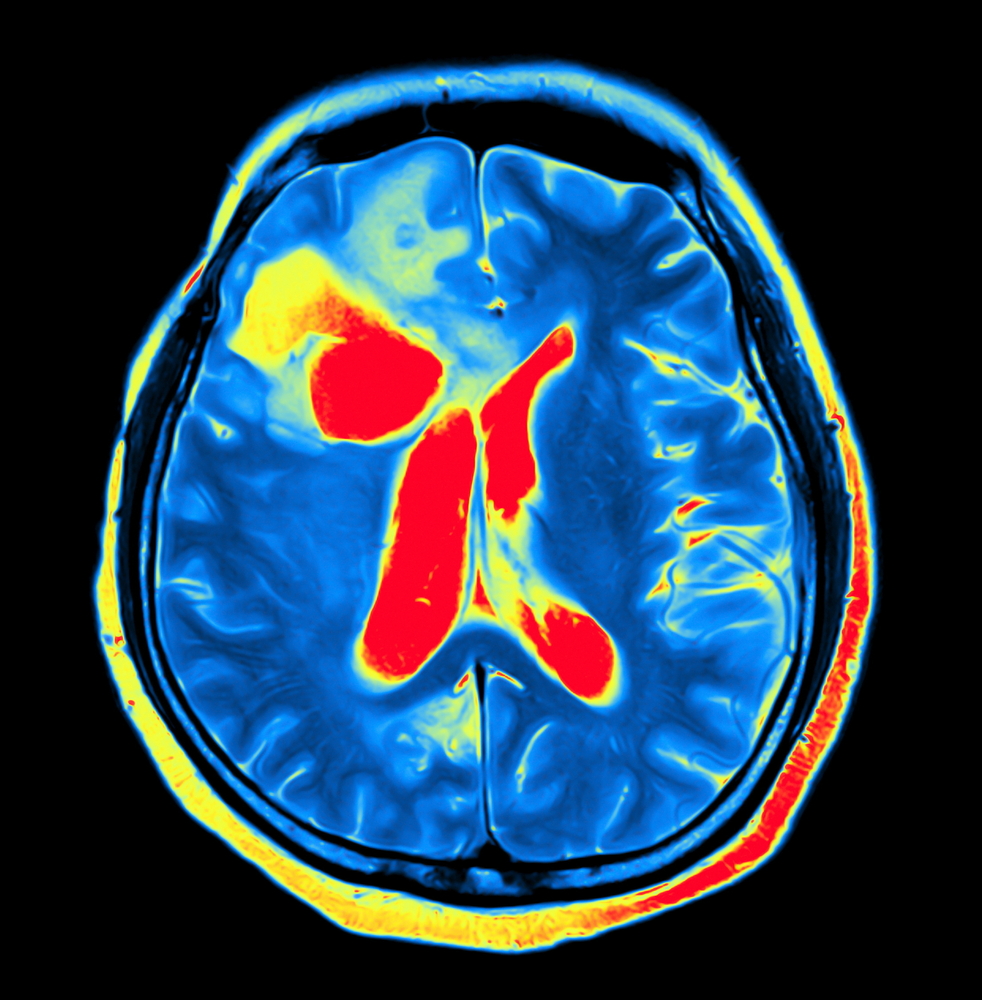
Parkinson’s disease is characterized by progressive deterioration of both motor and cognitive function, which is often treated with dopamine replacement therapy. Dopamine is a neurotransmitter that helps regulate movement as well as emotional responses. While dopamine therapy can help alleviate most motor symptoms, it can be complicated by a variety of adverse events, and half of Parkinson’s patients develop dyskinesias (involuntary muscle movement) within six years of starting treatment.
Dopamine medication can also lead to a range of cognitive abnormalities, including two specific behaviors — abuse of dopamine medication, known as dopamine dysregulation syndrome (DDS) and impulse control disorder (ICD). ICD includes behaviors such as excessive gambling or shopping, hypersexuality, and kleptomania.
There appears to be a conceptual similarity between behavioral disorders such as ICD and DDS and movement disorders such as dyskinesias: They are both a result of impaired volition, referring to the power to use one’s own will. While behavioral disorders are an impairment of cognitive volition, dyskinesia is an impairment of motor volition.
As these two disorders may theoretically share similar pathways, researchers hypothesized that dyskinesias may share similar markers with DDS and ICD, which would lend credence to the hypothesis that they have shared mechanisms.
That led researchers to perform a risk factor analysis for potential neuropsychiatric and/or motor markers of dyskinesias and DDS/ICD in a large cohort of patients with Parkinson’s disease.
Among the 654 patients studied, the DDS/ICD symptoms and dyskinesias were assessed using the Movement Disorders Society (revised) Unified Parkinson’s Disease Rating Scale. Researchers then picked potential associated variables and identified factors that were associated with DDS/ICD and/or dyskinesias.
Results showed that psychosis was found to be independently associated with cases of both dyskinesia and DDS/ICD.
Furthermore, other factors, including unpredictable motor fluctuations and depression, were independently associated with DDS/ICD, while the female gender, low tremor score, and high akinesia-rigidity score were associated with dyskinesia.
These results suggest that psychosis may be an important marker of impaired volition across both motor and cognitive domains.
“We suggest that clinicians ensure that patients who have begun to experience motor fluctuations are counseled on the addictive properties of dopaminergic medications and their potential for adverse behavioral effects,” the authors wrote.
“Similarly, dyskinesias should prompt evaluation for changes in neuropsychiatric status,” they added.





