KG Raphael
Forum Replies Created
-
Clinical trials with nicotine patches have shown that they are NOT effective for PD symptoms; if anything, they make you feel worse and can cause skin irritation. So, if you seem to experience short-term improvement, it is probably a placebo effect.
https://evidence.nejm.org/doi/full/10.1056/EVIDoa2200311
-
I am not sure WHY Botox injections into the salivary glands would work. Drooling in PD is thought to be caused by decreased swallowing frequency, not by an excess of saliva production.
-
Personal testimonials are hard to interpret. Randomized clinical trials are the way to go. Check this out:
<b itemprop=”name”>A Randomized Placebo-Controlled Study of a Transcranial Photobiomodulation Helmet in Parkinson’s Disease: Post-Hoc Analysis of Motor Outcomes
<b itemprop=”name”>J. Clin. Med. 2023, 12(8), 2846; https://doi.org/10.3390/jcm12082846
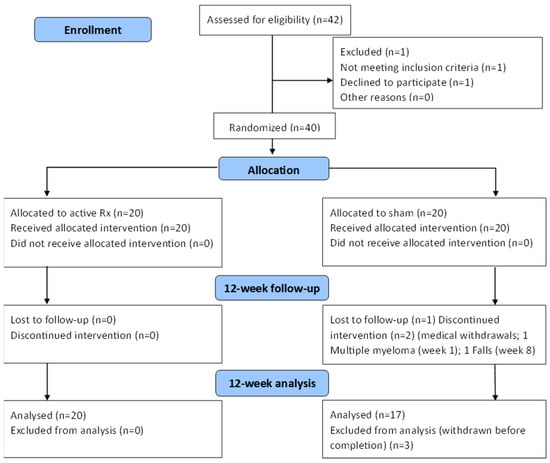
Emerging evidence is increasingly supporting the use of transcranial photobiomodulation (tPBM) to improve symptoms of neurodegenerative diseases, including Parkinson’s disease (PD). The objective of this study was to analyse the safety and efficacy of tPBM for PD motor symptoms. The study was a triple blind, randomized placebo-controlled trial with 40 idiopathic PD patients receiving either active tPBM (635 nm plus 810 nm LEDs) or sham tPBM for 24 min per day (56.88J), six days per week, for 12 weeks. The primary outcome measures were treatment safety and a 37-item MDS-UPDRS-III (motor domain) assessed at baseline and 12 weeks. Individual MDS-UPDRS-III items were clustered into sub-score domains (facial, upper-limb, lower-limb, gait, and tremor). The treatment produced no safety concerns or adverse events, apart from occasional temporary and minor dizziness. There was no significant difference in total MDS-UPDRS-III scores between groups, presumably due to the placebo effect. Additional analyses demonstrated that facial and lower-limb sub-scores significantly improved with active treatment, while gait and lower-limb sub-scores significantly improved with sham treatment. Approximately 70% of participants responded to active treatment (≥5 decrease in MDS-UPDRS-III score) and improved in all sub-scores, while sham responders improved in lower-limb sub-scores only. tPBM appears to be a safe treatment and improved several PD motor symptoms in patients that responded to treatment. tPBM is proving to be increasingly attractive as a possible non-pharmaceutical adjunct therapy.
doi.org
Emerging evidence is increasingly supporting the use of transcranial photobiomodulation (tPBM) to improve symptoms of neurodegenerative diseases, including Parkinson’s disease (PD). The objective of this study was to analyse the safety and efficacy of tPBM for PD motor symptoms. The … Continue reading
-
KG Raphael
MemberMarch 10, 2023 at 9:46 am in reply to: Can exercise delay Parkinson’s progression?Unfortunately, while personal experience can tell you whether you “feel better” after you exercise, there is no way that it can tell you whether your exercise regimen has changed the course of your PD progression. There is quite a bit of variability in progression of PD symptoms across individuals. You cannot know how you would being functioning long term without exercise. Believing that exercise slowed progression is not science; it is only belief.
Although review papers often incorrectly state that “exercise slows PD progression,” that is an unknown right now. There is a major confusion in the research literature and subsequent messaging to the public and people with PD: Yes, randomized controlled clinical trials of people with PD randomly assigned to (especially high intensity) exercise versus not assigned to similarly intensive exercise do score better on blind assessors’ ratings of motor symptoms as well as symptom self-ratings of health and symptoms. But are those temporary changes? Maybe but maybe not.
One would need to use a biomarker like DATScan, one strongly associated with disease progression. The multisite Northwestern Phase III SPARX3 trial plans to compare DATScans on individuals randomly assigned to high versus moderate intensity treadmill exercise for 18 months. For more information about participating, go to: https://www.sparx3pd.com/ . They are actively recruiting people with PD in 25 different locations throughout the USA (one site in Canada right now). Unfortunately, if you are currently exercising regularly now or taking PD meds, you are not eligible. More eligibility criteria can be reviewed at the website I link above. It’s a very important study; if you don’t qualify but know someone recently diagnosed who doesn’t regularly exercise, please refer them to the website.
-
KG Raphael
MemberJanuary 11, 2024 at 3:02 pm in reply to: Probiotic could ease Parkinson’s symptomsAfter all this fuss about mannitol… MOST people seem to stop taking it. The original positive evidence for mannitol was basaed on animal models. An Israeli entrepreneur with PD was frustrated about “undone science” where potentially helpful treatments were ignored by big pharma because there was no potential profit from over the counter treatment possibilities. Clinical trials are very expensive and it’s hard/competitive to get comparable funding from foundations or government sources like thh NIH.
The Israeli guy set up a crowd sourcing platform called Clinicrowd, where patients could report about their own exeriences with mannitol. In 2018, “more than 1500 Parkinson’s patients from 42 countries” had reported that they tried mannitol on the CliniCrowd platform. BUT only 78 people had continued to use it for more than 6 months as of 2018. Of those 78, 56% reported improvement. Not too impressive.
In late 2018, Hadassah Medical Center in Jerusalem funded a small clinical trial, in which people with PD were randomly and blindly assigned to receive either mannitol or dextrose (placebo). They reported no significant differences in outcome between the two groups.
The same thing with PS128 might be expected for PS128: The positive findings were from mouse or rat trials. Know that only humans get PD, so these are “induced” models of PD in animals. either through selective genetic breeding or through exposure to toxins that destroy the part of the brain containing dopaminergic neurons. It’s well known that findings from animal trials don’t replicate in humans. Rodents and all animals except our closest mammalian relatives don’t even have the same types of dopaminergic neurons as the ones that are vulnerable to dying in humans with PD, i.e., dopaminergic neurons containing neuromelanin (which makes them appear black, accounting for the black appearance of the substantia nigra part of the brain). Please don’t get too excited about promising symptom-relieving treatments from animal studies. Look for clinical trials in humans.
At this point, the only treatment other than standard PD medications that shows consistent evidence of symptom reduction in people with PD is EXERCISE. The more vigorous or intensive the exercise, the better!