Swedish Biobank Promises to Help Unveil Genetics of Parkinson’s
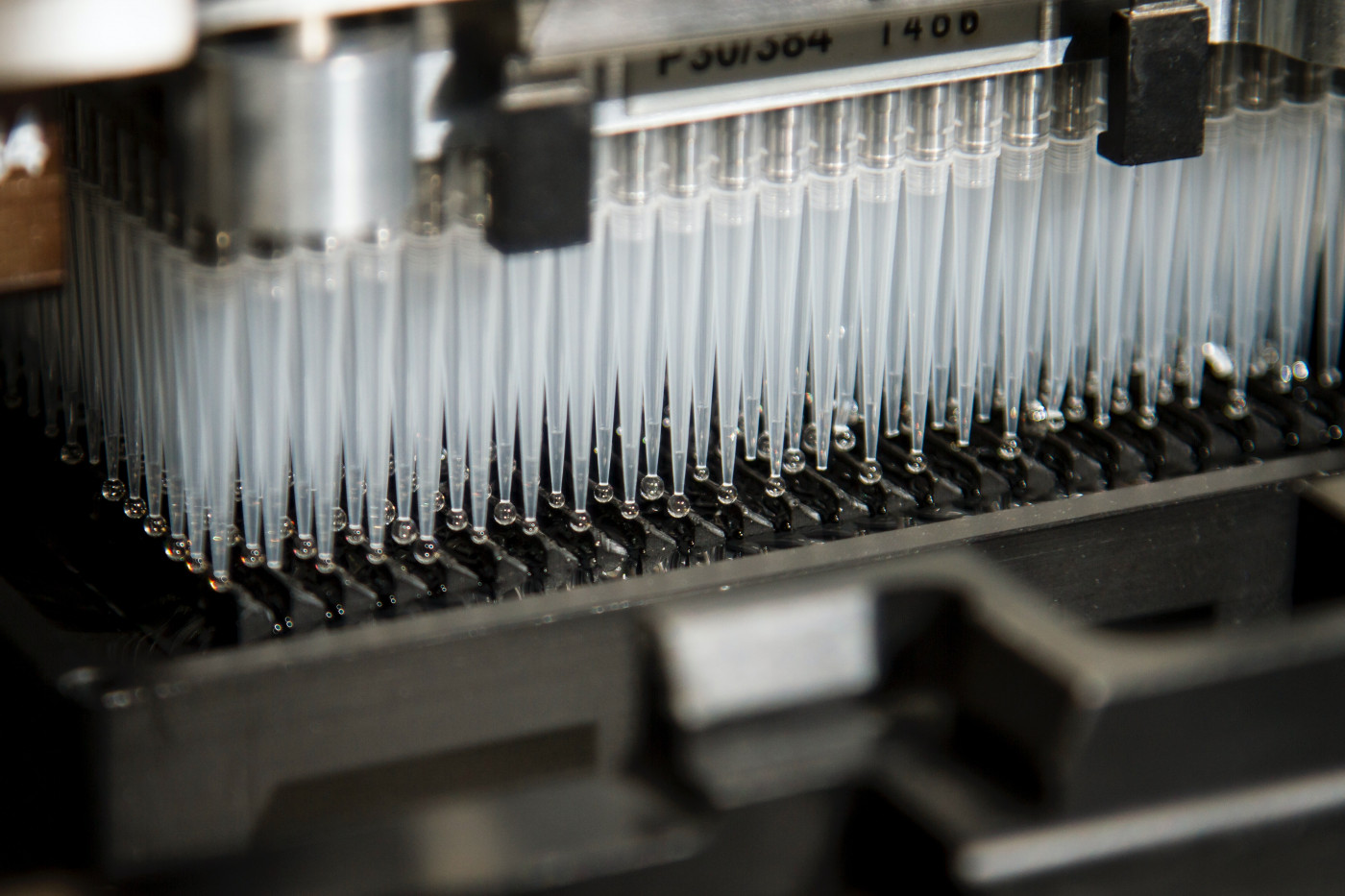
Stem cells
A new biobank in Sweden, containing blood samples from patients with Parkinson’s disease and age- and sex-matched healthy people — along with data regarding the individuals’ lifestyles and medical histories — may help researchers investigate the underlying mechanisms of the neurodegenerative disorder and find new treatments.
The biobank is part of the Multipark strategic research area at Lund University, in Sweden, and is the outcome of a four-year effort.
“I am convinced that many researchers will use the biobank over the next few years, which could lead to the development of new treatments,” Andreas Puschmann, MD, PhD, associate professor of neurology at Lund University Hospital, said in a university press release.
The biobank already has secured blood samples from half of all Parkinson’s patients — about 1,000 in total — in Skåne, a county in Sweden. An equally large control group also submitted blood samples. All of the participants answered a broad questionnaire “which captures everything from lifestyle factors, symptoms, course of the disease and use of medication,” the researchers said.
Besides plasma, which is the non-cellular component of blood, and serum — the portion of plasma remaining after coagulation of blood — the biobank also stores participants’ DNA and RNA. Of note, DNA is the genetic material found in all cells, while RNA is the molecule generated from DNA and used as the template for protein production.
The samples are stored deep-frozen underground in Lund’s Biobank Syd.
“We chose to take blood samples that enable many types of analysis depending on whether researchers in the future will want to look at biomarkers or genetic variations,” said Maria Swanberg, PhD, the biobank’s coordinator.
Additionally, all participants who agreed to give a sample to the biobank have responded to a questionnaire regarding their symptoms, disease course, and medication use. Answers also were recorded on questions about the participants’ lifestyles.
“The patient surveys we conducted enable the study of biomarkers and genetics in the blood and their connection with environmental factors. Access to the Swedish Parkinson’s register also enables patients to be monitored over time, and the study of their medical history and use of medication,” added Swanberg, who works as an associate professor of translational neurogenetics at Lund University.
Swanberg has studied lifestyle factors — such as coffee and tobacco use, and exposure to herbicides — and their potential role as risk factors for Parkinson’s disease.
The new biobank dataset can help researchers like Swanberg learn more about the role of environmental factors and possible disease risk.
“One strength of the case control study is that we see how it reproduces the known research results about Parkinson’s disease,” Swanberg said.
“As in several previous studies, we can observe that smokers and coffee-drinkers are affected to a lesser extent whereas exposure to pesticides increases the risk of the disease,” she said.
A 2019 study used data from the biobank — 658 DNA samples out of the total 2,206 analyzed — to investigate whether the most common genetic mutations linked to Parkinson’s were present in the Swedish population.
The results were surprising, as only 13 patients (0.6%) carried the most commonly reported mutations for which treatments are under development. Yet, the researchers found that a fraction of patients who carried these mutations had a relative with Parkinson’s disease, suggesting that other genetic factors are likely to play a role.
“It turned out that 21 percent of all patients had a relative with Parkinson’s, despite there being so few mutation carriers,” said Puschmann, the study’s lead author.
“We suspect that there is a significant genetic link to the disease, but that there may also be other underlying genetic factors and mechanisms,” he said. “Instead of a single gene, there may be an interaction between two or three genes.”
Many research groups are now trying to find which genes can contribute to Parkinson’s, and the new biobank, by providing both samples and patient information, could be an important tool to study this link.
“The RNA samples in the biobank enable researchers to observe the effect of the mutations on the genetic expression, for example. We will be able to do a lot in the next few years. Progress is being made step by step, which could lead to the development of new treatments,” Puschmannsaid.
“I am convinced that many researchers will use the biobank over the next few years, which could lead to the development of new treatments,” he added.
Kajsa Brolin, a PhD student at the translational neurogenetics lab at Lund University, is trying to understand why smokers are less likely to develop Parkinson’s compared with non-smokers.
To answer this, she is cross-referencing the biobank’s genetic information and lifestyle data.
“I combine data to see whether there is any connection between the nitrogenous bases, lifestyle habits and whether or not a person gets the disease. I conduct specific analyses on a group level but one can also use the biobank to examine the cell or protein level,” Brolin said.
Of note, nitrogenous bases are the building blocks, called adenine, cytosine, guanine and thymine, that compose the DNA molecule.
When asked about what, in her opinion, is the biobank’s contribution for future research, she said “to understand the disease.”
“The main focus is on the genetic causes of the disease and on understanding the underlying biological processes,” Brolin said.
“The big objective is to find new drugs; I hope that the biobank can be one piece of that particular puzzle,” she said.
In the future, Multipark wants to include its biobank in studies done by the International Parkinson’s Disease Genomics Consortium, the Global Parkinson’s Genetic Programme, and others.






