Deep-brain Stimulation Can Reverse Mitochondria Defects Linked to PD, Study Finds
Deep brain stimulation therapy can help lessen Parkinson’s symptoms, partly by increasing the number of mitochondria — cells’ powerhouses — in brain nerve cells, a study shows.
The study, “Post mortem examination of Parkinson’s disease brains suggests decline in mitochondrial biomass, reversed by deep brain stimulation of subthalamic nucleus,” was published in The FASEB Journal.
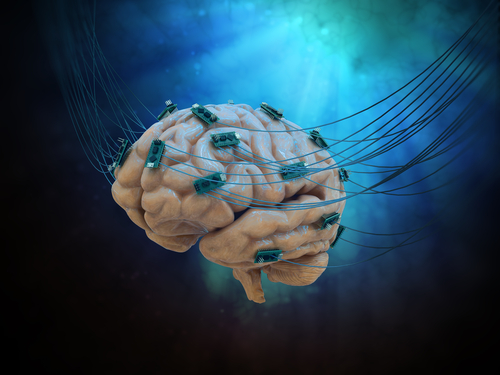
DBS is an invasive technique in which thin wires are surgically implanted into the brain to deliver electric pulses to specific brain areas and ease motor symptoms, such as tremors, in patients for whom standard medications are not effective.
Studies have shown that DBS can effectively reduce motor symptoms and the necessary daily dose of medication, improving quality of life both in patients with advanced Parkinson’s and those with early-stage disease.
However, despite being the most commonly used surgical treatment for Parkinson’s disease, the exact mechanisms through which DBS may work to help prevent nerve cells’ degeneration remain elusive.
Now, researchers at the Imperial College London analyzed brain cells collected from individuals with Parkinson’s disease who had either received DBS (three patients) or not (four patients), as well as from three healthy individuals. All the tissue samples were collected post mortem and had been stored at the Parkinson’s UK Brain Bank, at the Imperial College London.
Want to learn more about the latest research in Parkinson’s Disease? Ask your questions in our research forum.
The team found that Parkinson’s-affected brain cells had fewer mitochondria compared to healthy ones. Also, the mitochondria were not located inside the cells where they normally are, such as the synaptic terminals. Synapses are junctions between two nerve cells that allow them to communicate.
“These results suggest a change in the availability of mitochondria in synaptic terminals as a precursor or a result of Parkinson’s disease,” researchers said.
Samples from patients who had undergone DBS had fewer mitochondria than control samples, but slightly more than Parkinson’s patients not treated with DBS. In addition, the volume of these energy-producing organelles in DBS-treated samples was closer to that observed in healthy brain cells.
“DBS treatment seemed to have inhibited or reversed the reduction in mitochondrial volume and numbers caused by Parkinson’s disease,” researchers wrote. These results suggest “enhanced metabolic plasticity leading to neuroprotection” in the brain areas most affected by the disease as a result of DBS.
Additional studies are still warranted to better understand the effects of DBS therapy on mitochondria and overall nerve cell survival.
“This potentially opens avenues for exploring how to replicate this cell power-up with non-surgical treatments, without the need for implanting electrodes in the brain,” Kambiz Alavian, PhD, lecturer in the department of medicine at the Imperial College London and senior author of the study, said in a news release written by Kate Wighton.
Brain tissue samples are one of the most reliable sources of information on neurological disorders. However, studies using this type of sample can be challenging, as they can only be performed after an individual has died.
“We now hope to carry out larger studies to explore new treatments that may preserve brain cell mitochondria. The ultimate goal would be to keep cells powered up for longer, and Parkinson’s symptoms at bay,” he said.