Engineered Protein May Lead to New Parkinson’s Therapy, Preclinical Study Suggests
A modified form of a protein called Nurr1 that is able to protect against nerve cell death and restore dopamine production in a preclinical setting may pave the way for a possible new Parkinson’s therapy, a study reports.
The study, “Lethal Factor Domain-Mediated Delivery of Nurr1 Transcription Factor Enhances Tyrosine Hydroxylase Activity and Protects from Neurotoxin-Induced Degeneration of Dopaminergic Cells,” was published in the journal Molecular Neurobiology.
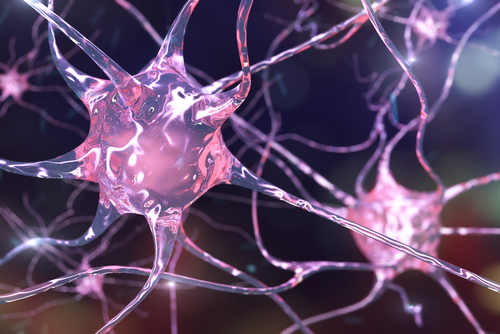
The nuclear receptor-related 1 protein, or Nurr1, plays a role in the development and survival of dopamine-producing neurons in the brain, a cell population that progressively degenerates in Parkinson’s disease, leading to lower dopamine levels.
As a type of protein called a transcription factor, Nurr1 controls the production of other key proteins in these neurons, while also regulating apoptosis, or “programmed” cell death.
An age-dependent reduction in Nurr1 levels has been proposed as one of the causes behind the loss of dopamine-producing neurons in Parkinson’s patients. Preclinical work showed that elevated levels of this protein provide anti-inflammatory benefits and neuroprotection.
Gene therapy approaches to deliver Nurr1 into animals and administration of compounds designed to boost its effects have shown promising results, but the protein’s inability to enter cells and reach their nucleus has remained a limitation for the potential development of therapies.
But now researchers from Ruhr Universitat Bochum in Germany and the U.S. National Institute of Allergy and Infectious Diseases at the National Institutes of Health have found a way to modify Nurr1 with a nontoxic bacterial protein fragment, a similar mechanism by which Bacillus anthracis infiltrates animal cells and causes anthrax, to help it get where it needs to go. A protein known as SUMO was also used to increase Nurr1’s stability.
“The fragment of bacterial protein that we used does not trigger diseases; it merely contains the command to transport something into the cell,” Rolf Heuman, one of the study’s authors, said in a press release.
After it is taken up by the cell, the protein fragment is detached, and Nurr1 is then able to reach its target genes by using the cell’s own nuclear import machinery.
Want to learn more about the latest research in Parkinson’s Disease? Ask your questions in our research forum.
Using human dopamine-producing cells grown in the laboratory, researchers found that successful delivery of modified Nurr1 was associated with higher levels of an enzyme called tyrosine hydroxylase, the key enzyme in dopamine production.
The team also tested the effect of modified Nurr1 on the cultured cells treated with the neurotoxin 6-hydroxydopamine, which causes the dopamine-producing cells to die and is used as a model for Parkinson’s. Nurr1 was able to inhibit the neurotoxin-induced degeneration of cells.
“Nurr1 fusion protein may contribute to the development of a novel concept of protein-based therapy,” the researchers wrote in the study.
Current Parkinson’s medications are not able to restore dopamine-producing neurons or stop their degeneration. A different approach, deep brain stimulation, has been effective in easing motor symptoms, but still carries safety risks.
“We hope we can thus pave the way for new Parkinson’s therapy,” said Sebastian Neumann, the study’s senior author. “Many steps still remain to be taken in order to clarify if the modified protein specifically reaches the right cells in the brain and how it could be applied.”